Emergency Medicine: Quality Improvement
Emergency Medicine 5 B
334 - "The Effect of Protocolized Intravenous Hydration in Reducing the Rate of Urinary Catheterization in Girls Undergoing Pelvic Ultrasound in the Emergency Department"
Publication Number: 334.209

Navid Anvaripour, MD (he/him/his)
Resident
Driscoll Children's Hospital
Corpus Christi, Texas, United States
Presenting Author(s)
Background:
A urine-filled bladder is a requirement for Pelvic ultrasound in females. At Driscoll Children's Hospital, the standard of care was placement of Foley catheter to fill the bladder with normal saline prior to pelvic Ultrasound.
Objective:
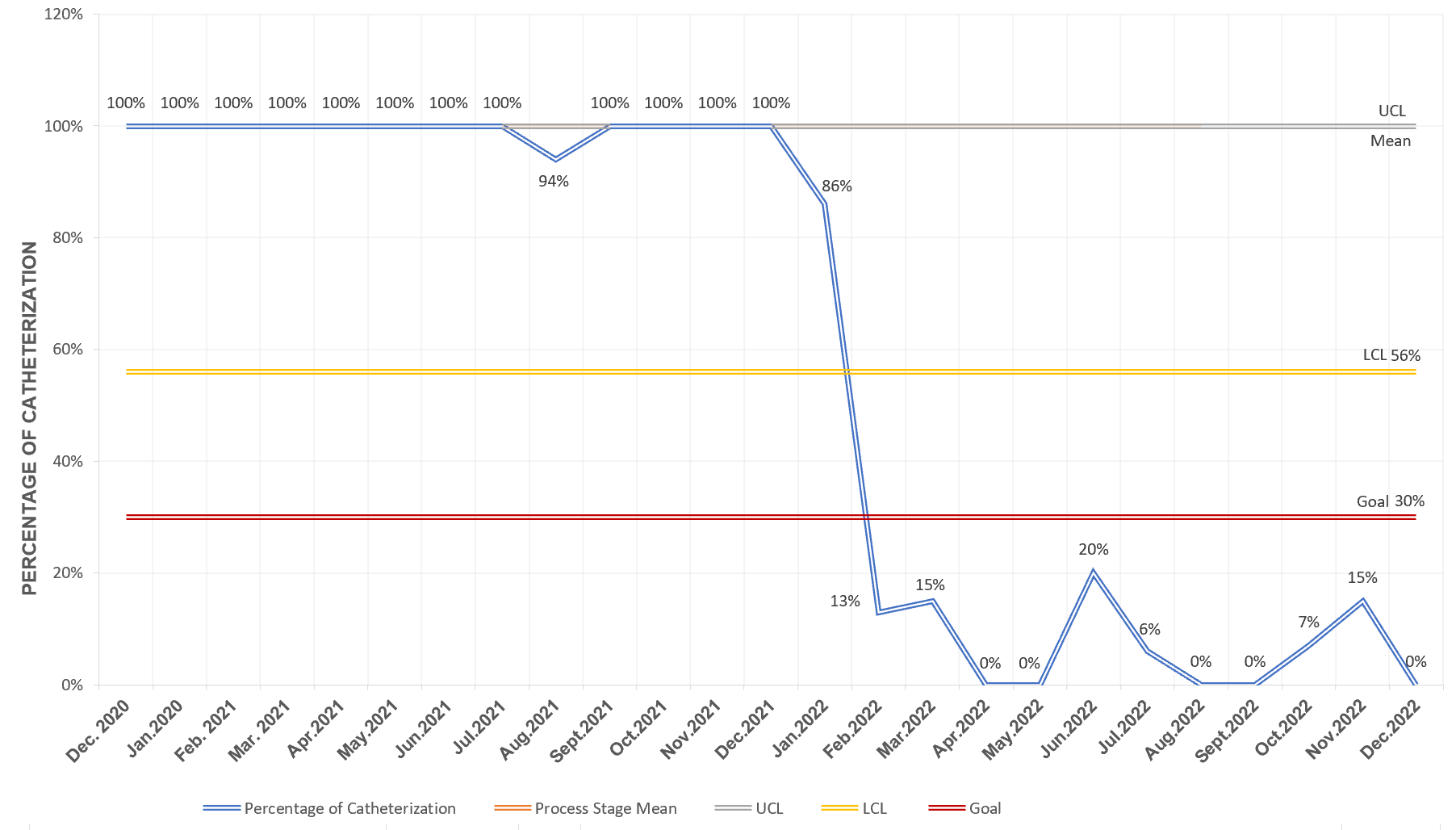
Decreasing the rate of urinary catheterization in girls between the ages of 12 to 20 years, for whom pelvic ultrasound is ordered in the Emergency Department, from the baseline rate of 100%, to 70% over 6 months and thereafter, decrease the rate by 10% every 3 months, over the next 12 months and maintain or improve this rate for 2 years afterwards
Design/Methods:
After several meetings with the team members prior to the study, we designed a Key Driver Diagram to help us to overcome the barriers to implementation and we created a flowchart as a guide for the ED providers. We started the QI project on 1/25/2022. We have had 3 team member meetings since the QI project began, where we studied and improved upon our three PDSA cycles.
We used a clinically indicated and already established IV line and hydration to fill the bladder. According to our flow chart, we used bladder scan to measure the bladder urine volume right after a pelvic ultrasound was ordered; given the present urine volume, we followed our flowchart for the IV infusion of normal saline to fill the bladder to the optimal amount necessary for pelvic ultrasound based on the Koff Formula.
Results:
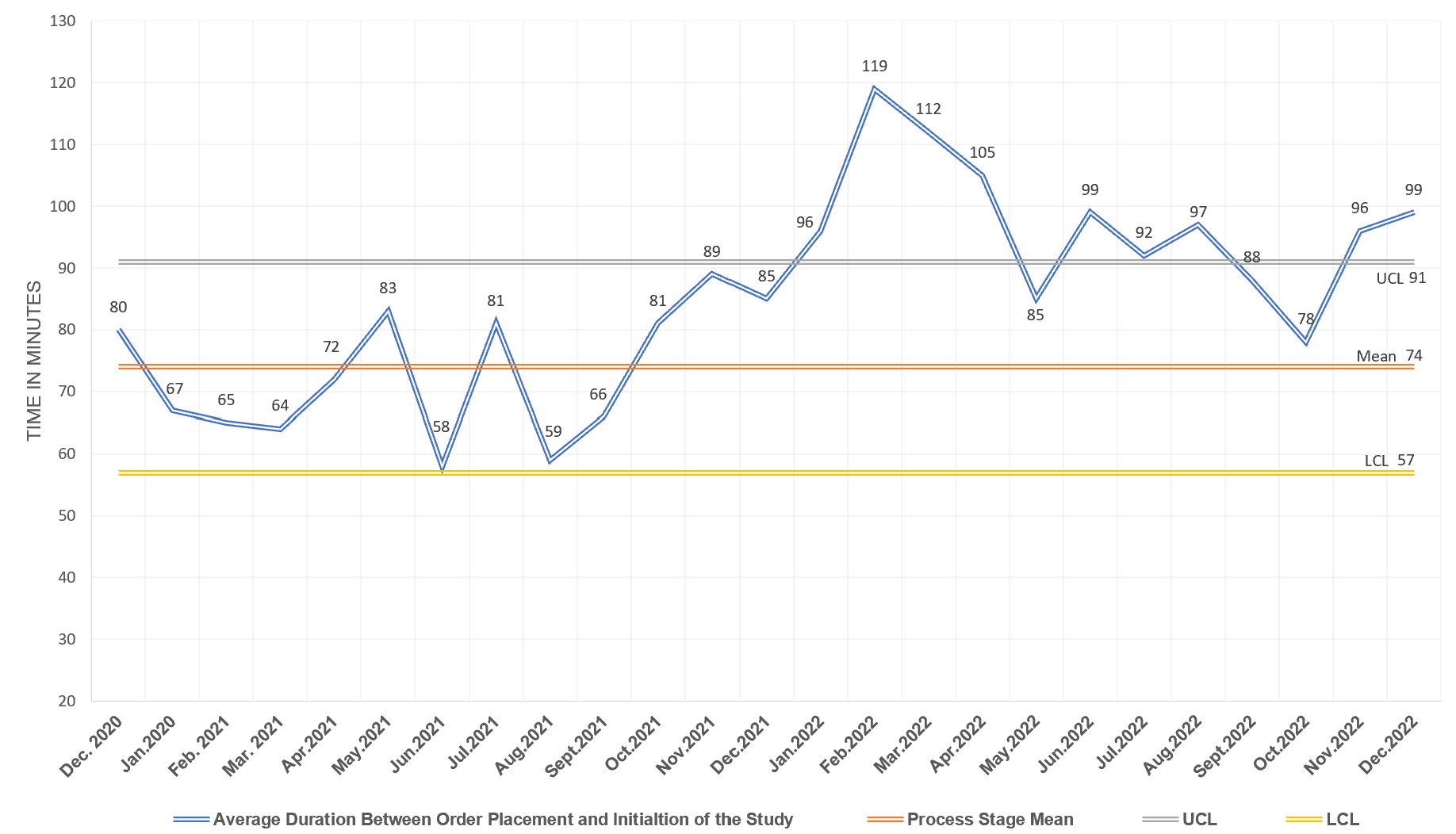
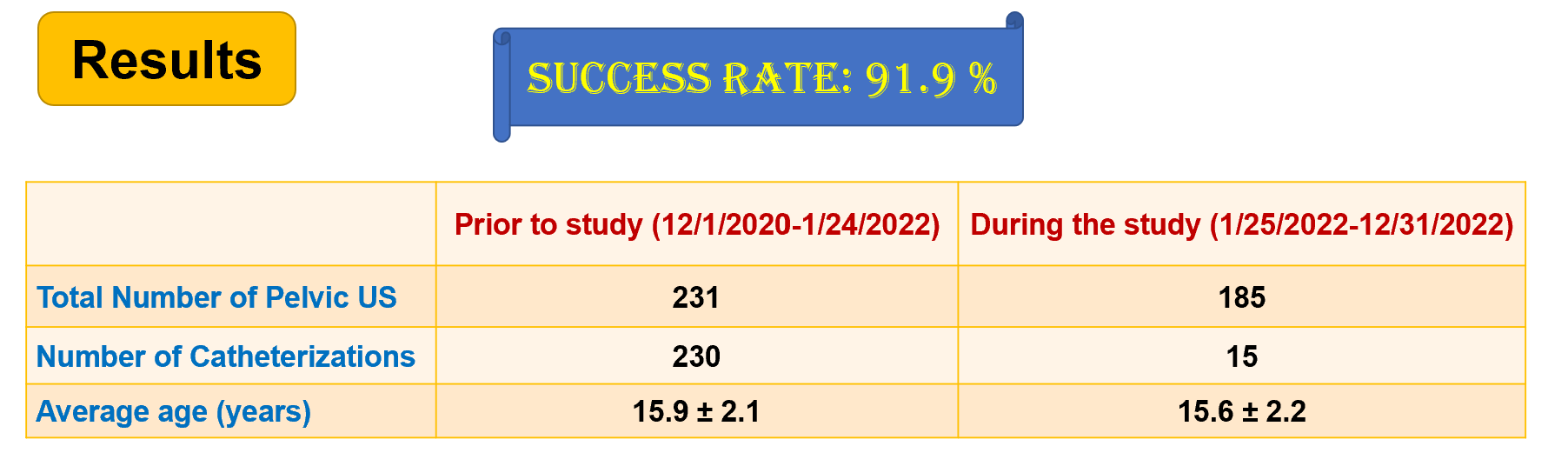
Since 1/25/2022, 196 pelvic ultrasounds were ordered in our ED for our study population; eleven patients had emergency situations that required immediate pelvic ultrasound and surgical intervention and were excluded from the study. Of the remaining 185 patients, only 15 patients underwent Urinary catheterization, resulting in a significant decrease in the rate of catheterization, from the baseline of 100% to 8.1%. Although we accomplished the goal of the QI project, there was an increase in delay between ultrasound order placement and pelvic ultrasound, from a baseline of 74 minutes to 98 minutes.
Conclusion(s):
With the initiation of the improvement project in our ED, there was a noticeable decrease in the percent of patients catheterized. This goal was achieved while meeting patient's and parents' satisfaction, with less burden on our nurses and staff, and without any observed side effects. By following this QI project and maintaining this success rate, we prevent potential side effects and negative psychological impacts on patients. Although a mild delay of care was observed during our improvement project, it has not caused any harm to the patients, and we will study additional PDSA cycles to eliminate the delay.