Emergency Medicine: Quality Improvement
Emergency Medicine 5 B
340 - Improving Emergency Department Throughput During Viral Surge in a New Satellite Pediatric Emergency Department
Publication Number: 340.209

Naomi Hughes, MD (she/her/hers)
Assistant Clinical Professor of Pediatrics, Perelman School of Medicine, University of Pennsylvania
Childrens Hospital of Philadelphia
Philadelphia , Pennsylvania, United States
Presenting Author(s)
Background:
Our institution opened a satellite pediatric hospital site in January 2022, with a 20-bed emergency department (ED) and predicted volume of 23,000 ED patients/year. The viral season of 2022 strained our system resulting in high numbers of patients leaving without being seen reaching as high as 28% We describe our quality improvement efforts to approach this problem through monitoring data and making iterative changes to improve ED throughput and improve access to care for our community.
Objective:
We used a quality improvement framework to identify interventions to improve ED throughput with an aim to achieve and maintain a left without being seen (LWBS) rate of < 1.6%.
Design/Methods:
We analyzed the problem of high LWBS rates by identifying primary and secondary drivers causing delays in ED throughput.(Figure 1) Several change concepts were identified and we implemented feasible changes both locally with our ED by increasing space and staffing resources, as well as outside the ED with enterprise-wide efforts. We monitored many throughput metrics, including LWBS rate, number of patients presenting, and number of patients waiting in the ED for an inpatient bed longer than 4 hours from bed request (High Occupancy Hold(HOH)).
Results:
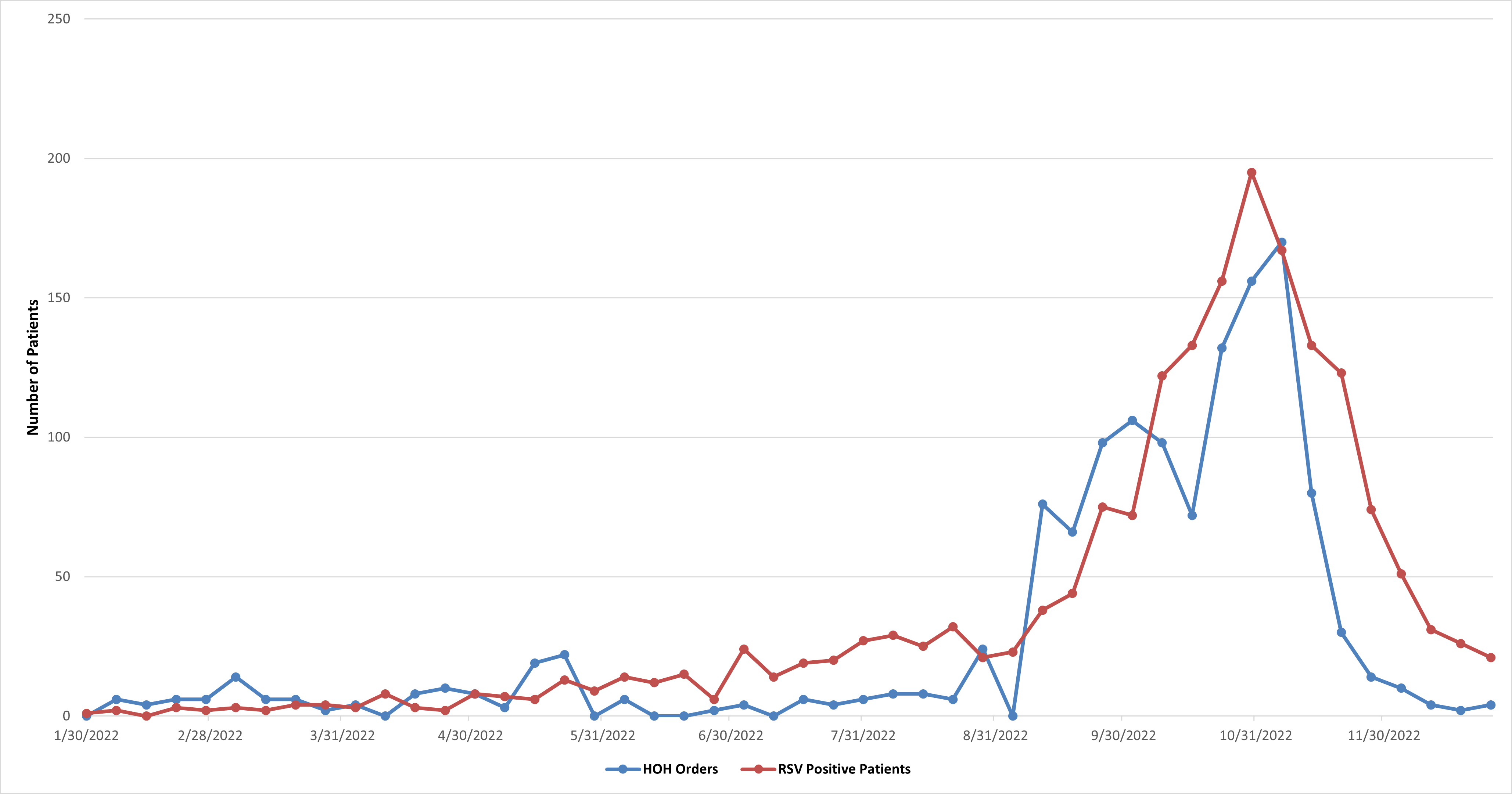
The SPC chart of LWBS rates in figure 2 demonstrates centerline shifts in negative and positive directions, correlating with Respiratory Syncytial Virus (RSV) noted in figure 3. Our interventions are listed in figure 2. The biggest drop in LWBS rates coincided with implementation of a hospital wide effort increasing inpatient capacity and decreasing HOH patients in the ED, the opening of a surge space to care for ED patients, as well as a decrease in number of patients with RSV. Figure 3 shows that the drop in number of HOH patients preceded the drop in number of RSV patients during the last two weeks of November.
Conclusion(s):
The emergency department is uniquely positioned to identify when adequate access to health care is threatened. Our LWBS rate was significantly impacted by the increase RSV in our community. There is a point in which restructuring resources within the ED alone is not sufficient to provide adequate ED throughput. We were ultimately able to provide an enterprise-wide response that incorporated shifts in resources across a larger system to improve access to ED care more rapidly than restructuring resources within the ED alone. Identifying when ED resources are inadequate and initiating a system wide response would be helpful in the future to allow continued access to high quality ED care by maintaining ED throughput and keeping LWBS rates below 1.6%.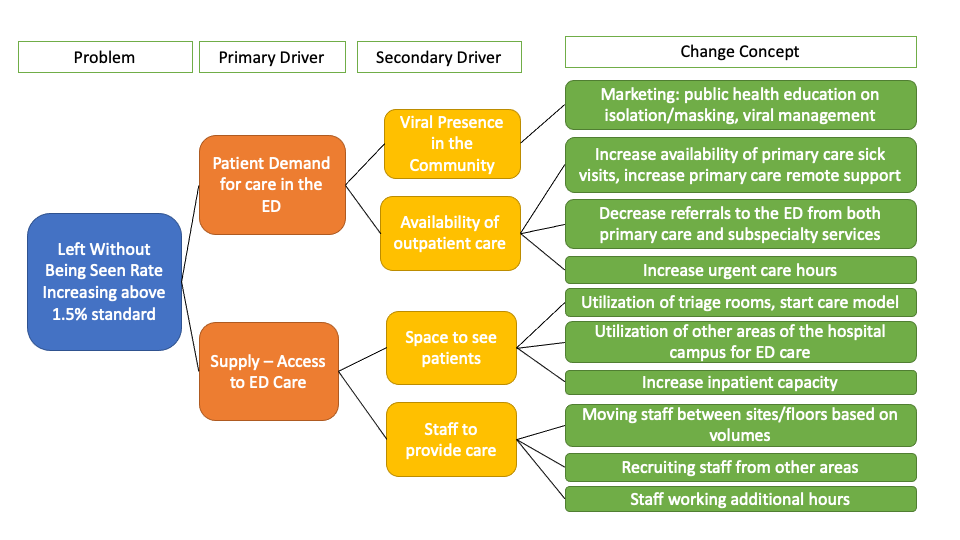
.png)