Medical Education: Resident
Medical Education 7: Resident 2
541 - A Multi-Site Collaborative Contributes to Resident Knowledge, Skills, and Attitudes for Addressing Food Insecurity
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 541
Publication Number: 541.229
Publication Number: 541.229
Emily B. Vander Schaaf, University of North Carolina at Chapel Hill School of Medicine, Carrboro, NC, United States; Laurie W. Albertini, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States; Jeffrey P. Holloway, University of South Carolina School of Medicine Greenville, Columbia, SC, United States; Meredith Eicken, University of South Carolina School of Medicine Greenville, Greenville, SC, United States; James Roberts, Medical University of South Carolina, Charleston, SC, United States; Debra Best, Duke University School of Medicine, Durham, NC, United States; Margaret Ellis, Atrium Health, Charlotte, NC, United States; Stefanie Reed, Wake forest school of medicine, Charlotte, NC, United States; Lizmarie Maldonado, Medical University of South Carolina, Charleston, SC, United States; J. Blakely Amati, Prisma Health/University of South Carolina School of Medicine Greenville, Greenville, SC, United States; Elizabeth Erickson, Duke Children's, Durham, NC, United States; Karin Hillenbrand, Brody School of Medicine at East Carolina University, Greenville, NC, United States

Emily B. Vander Schaaf, MD, MPH, FAAP (she/her/hers)
Associate Professor
University of North Carolina at Chapel Hill School of Medicine
Carrboro, North Carolina, United States
Presenting Author(s)
Background: A 2021 survey demonstrated that many pediatric residents, including those at graduation, feel unprepared to screen and especially offer resources for food insecurity (FI), suggesting graduates may identify problems they are not prepared to address.
Objective: Evaluate the effect of an 8-site collaborative’s education and quality interventions on resident knowledge, skills, and attitudes about addressing FI
Design/Methods: The Carolinas Collaborative brought together the 8 pediatric residency programs in North and South Carolina with a unified goal to address FI. All sites engaged residents in local quality improvement projects to improve FI screening and referrals via shared curricular resources and best practices for FI education. Residents across all sites completed baseline and follow up surveys assessing knowledge, skills, and attitudes about screening for and addressing FI. Analyses were chi-square, Fischer’s exact test, or Kruskal-Wallis, as appropriate.
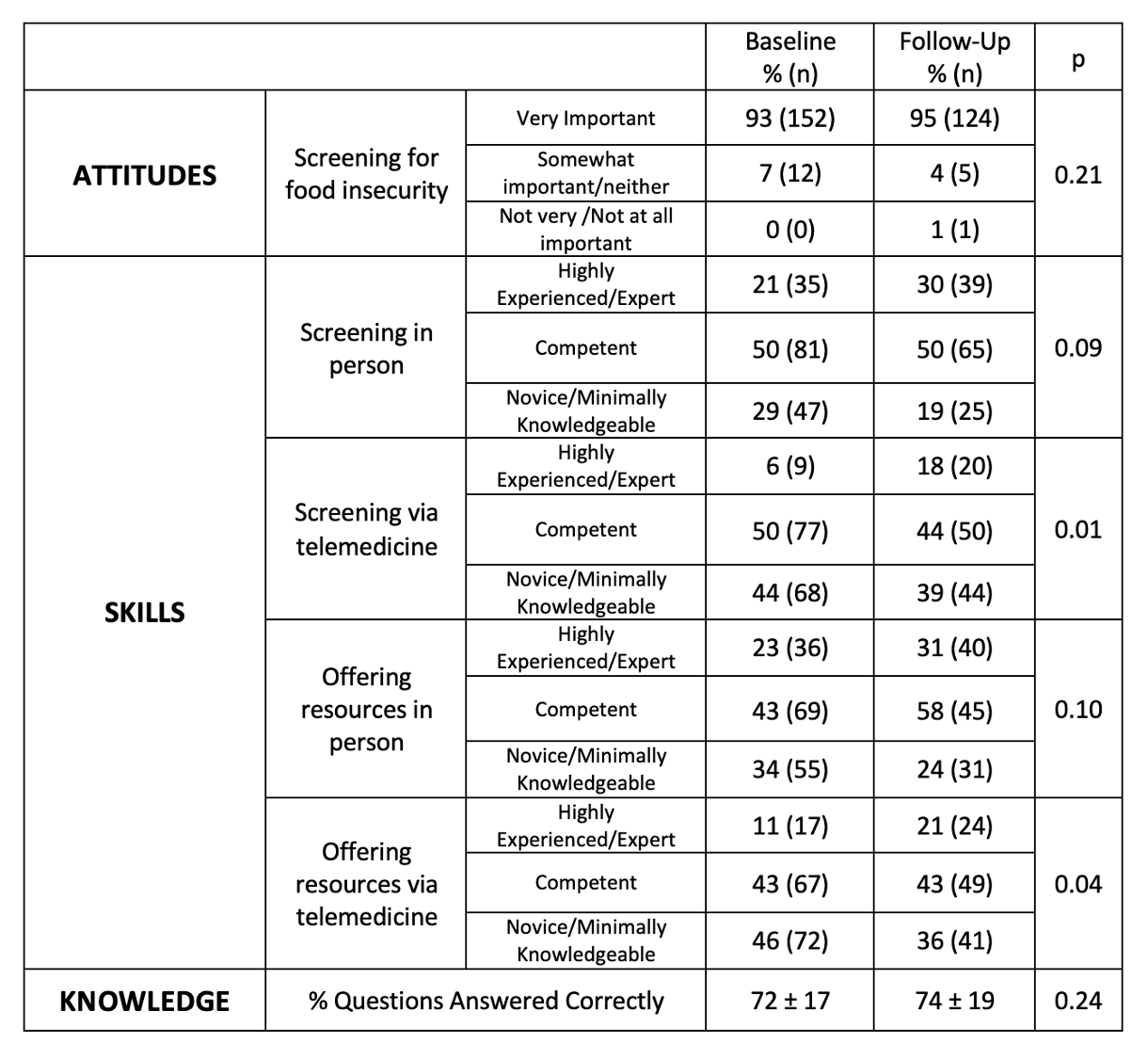
Results: 130 (31%) of invited residents completed the survey at follow up compared with 160 (38%) at baseline; a similar proportion completed it from each institution at baseline and follow up. At both timepoints, nearly all residents highly valued screening for FI in clinical settings (95%) and senior residents had better skills and knowledge about screening and offering resources than interns. From baseline to follow up, there was a decrease in those reporting feeling novice when screening (29 vs 19%, p=0.06) and offering resources (46 vs 36%, p=0.06) in person, as well as in screening (44 vs 39%, p=0.36) and offering resources (46 vs 36%, p=0.09) via telemedicine. Comparing trainees by year, third and fourth-year residents demonstrated the most improvement at follow-up compared to baseline, with only 13% reporting novice skills when offering resources compared with 33% at baseline (p=0.03). Likewise, more final year residents at follow-up than at baseline felt they had had adequate training in screening for FI (82 vs 56%, p=0.03) and in offering FI resources (74 vs 51%, p=0.05).
Conclusion(s): A multisite collaborative effort improved residents’ skills addressing FI, enhanced perception they had received enough training, and improved residents’ ability to connect families with resources, particularly graduating residents. These residents may be more prepared to identify FI and to meet their patients’ FI needs when they enter practice, potentially improving health outcomes. Future studies should measure durability of change over time, and assess outcomes for the populations served.
.jpg)
