Medical Education: Simulation & Technology
Medical Education 6: Simulation & Technology 1
526 - A Pilot Test of Expert Neonatal Resuscitation Teams’ Perceptions and Experiences of Mixed Reality Simulation
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 526
Publication Number: 526.228
Publication Number: 526.228
Mary C. Ottolini, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Michael Ferguson, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Micheline Chipman, Hannaford Center for Safety Innovation and Simulation, Pownal, ME, United States; Sarah Gabrielson, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Mark Griswold, Case Western Reserve University School of Medicine, Cleveland, OH, United States; Leah Mallory, Maine Medical Center, Hannaford Simulation Center, Portland, ME, United States; Michael Zubrow, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; ALLISON ZANNO, MAINE NEONATOLOGY ASSOCIATES, PORTLAND, ME, United States; Misty Melendi, The Barbara Bush Children's Hospital at Maine Medical Center, Portland, ME, United States; Kristin Greenwood, Northeastern University, Boston, MA, United States
- MO
Mary C. Ottolini, MD, MPH, MEd (she/her/hers)
Department Chair
The Barbara Bush Children's Hospital at Maine Medical Center
Portland, Maine, United States
Presenting Author(s)
Background: Rural hospital neonatal resuscitation teams may go months between deliveries requiring resuscitation, leading to disparities in newborn outcomes at small, rural hospitals compared to tertiary care centers. Financial and resource barriers in rural areas limit access to high-fidelity (HF) simulation for deliberate practice. Mixed reality (MR) provides a possible innovative solution to address rural simulation training needs.
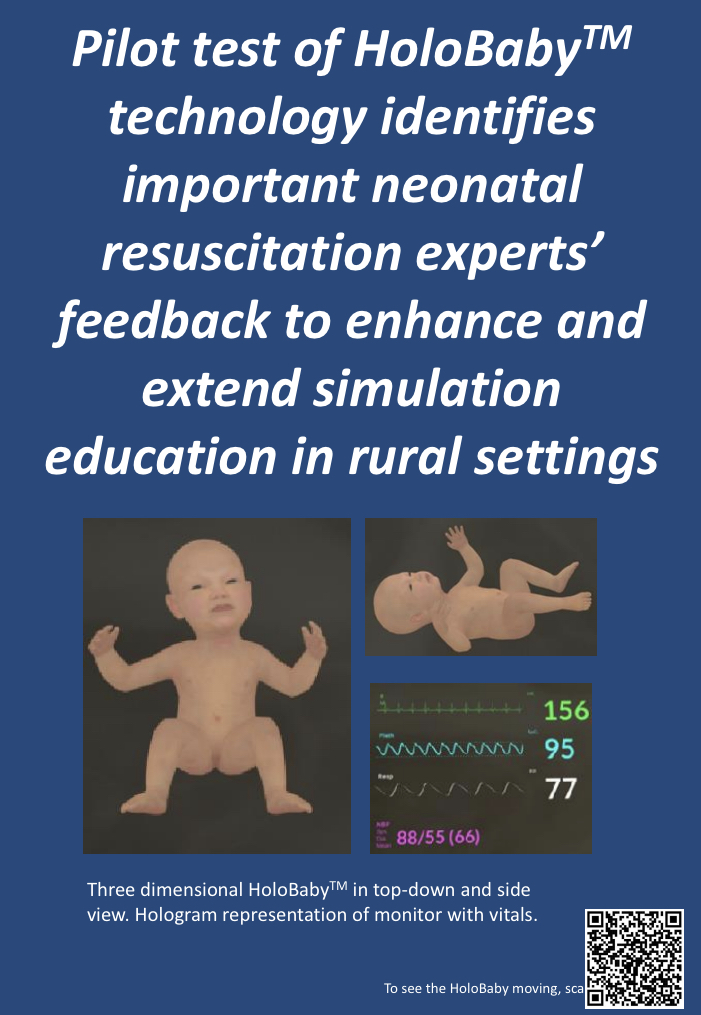
Objective: To determine expert perspectives of "HoloBaby" TM, a novel MR simulation technology compared to HF neonatal simulation.
Design/Methods: We created "HoloBaby"TM an application depicting a holographic representation of a neonate in distress projected onto an inexpensive manikin using a "HoloLens 2" for team training. The HoloBaby's physical and physiologic state can be changed based upon varied scenarios and the actions of team members during the simulation analogous to a HF manikin. We then recruited a convenience sample of 13 interprofessional clinicians from a Level IV NICU with HF experience. Subjects participated in a known HF simulation followed by a MR simulation utilizing the HoloBabyTM. We used a mixed methods design to collect expert perceptions of MR compared to HF using post-simulation surveys and focus groups.
Results: Qualitative analysis of focus groups revealed the following 3 themes:
Opportunities for enhanced reality over HF simulation with refinement.
Expectations of MR mismatch MR experience.
Training and education needed to account for cognitive load adjustments.
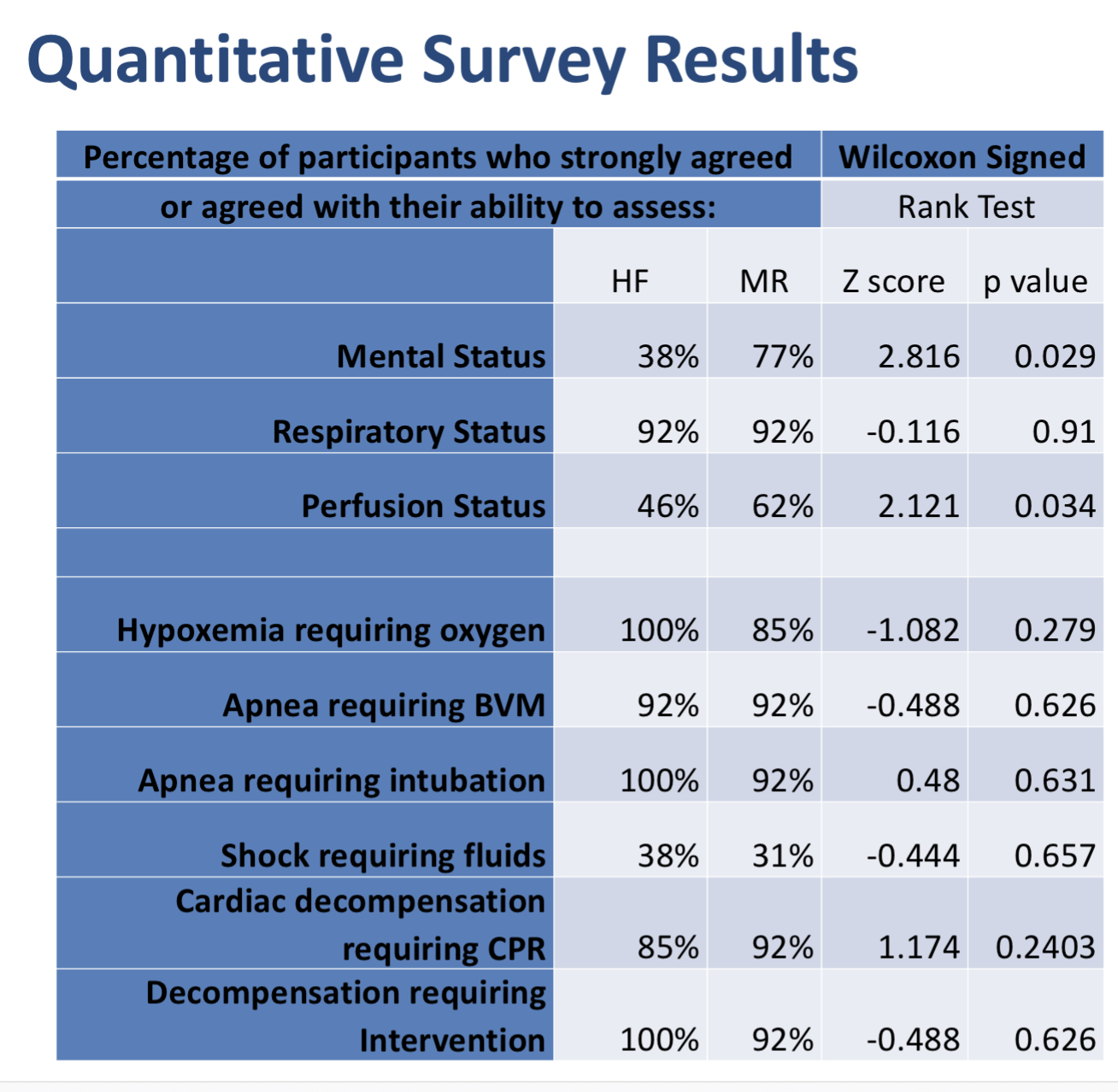
Quantitative survey results are shown in Table 1.
Conclusion(s): We identified limits and opportunities for HoloBabyTM technology to enhance simulation education and extend to rural settings. Consideration of cognitive load on performance and the need to practice with HoloLens technology merit further investigation. HoloBabyTM matched or exceeded high-fidelity manikin experience in the fields of realism tested. HoloBabyTM demonstrated promise to offer a training in a resource poor setting.