Hospital Medicine: Education
Hospital Medicine 3
496 - The Impacts of a Resident Clinical Documentation Improvement Curriculum
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 496
Publication Number: 496.221
Publication Number: 496.221
Camille Carre, University of South Florida Department of Pediatrics, Saint Petersburg, FL, United States; Diana Young, Johns Hopkins All Children's Hospital, Tampa, FL, United States; Paola B. Dees, Johns Hopkins All Children’s Hospital, Saint Petersburg, FL, United States; Tasnia Osmani, Tampa General Hospital Children's Medical Center, Tampa, FL, United States; Nikhil Bhatia, USF Health, Tampa, FL, United States
- CC
Camille Carre, MD (she/her/hers)
Chief Resident
University of South Florida Department of Pediatrics
Saint Petersburg, Florida, United States
Presenting Author(s)
Background: “Systems based practice” is part of the six core competencies for resident education by the Accreditation Council for Graduate Medical Education (ACGME). Knowledge of appropriate coding terminology is essential for tracking metrics for patient safety and quality. Although residents are the primary author for clinical documentation, studies show around 40% have little to no knowledge of CDI. Baseline data at Johns Hopkins All Children’s Hospital (JHACH) show residents have only a 75% accuracy at choosing appropriate diagnostic terminology for malnutrition. We created a CDI curriculum based on ten commonly queried documentation diagnostic codes, including malnutrition, to educate residents.
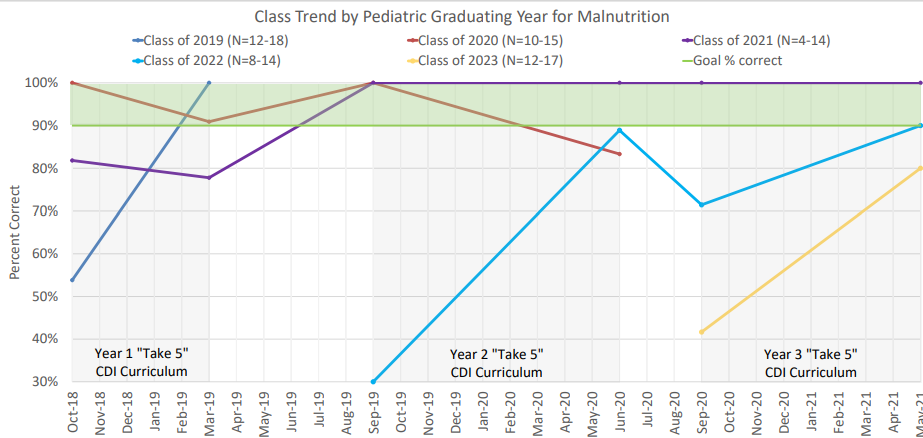
Objective: Our objective was to use the CDI curriculum we created for pediatric residents on the pediatric hospital medicine service to educate residents on the accurate identification and documentation of malnutrition. Our aim was to improve resident knowledge in proper documentation of malnutrition from 75% to at least 90% from October 2018 to June 2020.
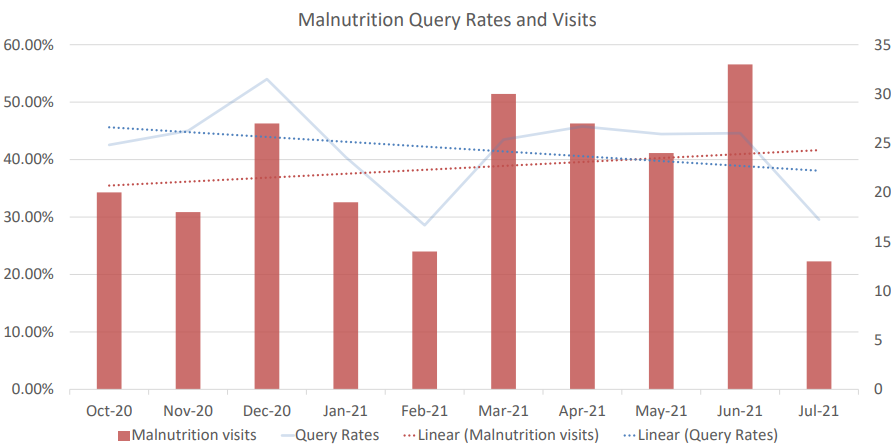
Design/Methods: Pediatric residents were assessed on their ability to accurately document malnutrition on anonymous "pre-surveys". Throughout the year 5 academic lectures were given on 10 commonly queried documentation diagnostic codes including malnutrition. At the completion of the curriculum residents were again assessed on their ability to properly document malnutrition on anonymous "post-surveys". Our primary measure was the percentage of residents who correctly answered our malnutrition question. Our secondary outcome is malnutrition query rates.
Results: We found that 76% of surveyed pediatric residents were able to accurately identify proper documentation terminology for malnutrition in the 2018-2019 academic year. Overall, the classes of residents showed an improvement over the course of 3 years. The class of 2021 and 2022 showed a sustained improvement and were able to meet the 90% threshold by the end of the study period. Our secondary outcomes showed that while patients admitted with malnutrition increased, query rates actually decreased from 10/2020 to 7/2021.
Conclusion(s): Our study shows that a CDI curriculum directed at residents can improve resident's knowledge in proper documentation terminology of malnutrition. Our study did have significant data variability which was likely due to smaller sample size and different residents being surveyed over the course of 3 years.