Infectious Diseases
Infectious Diseases 1
622 - Placental thrombosis resulting in hypoxic ischemic encephalopathy in an infant of a mother with COVID-19
Publication Number: 622.225

Kathleen Tedesco, MD (she/her/hers)
Resident PGY3
LAC+USC Medical Center/Keck School of Medicine of the University of Southern California
Los Angeles, California, United States
Presenting Author(s)
Background:
Since the beginning of the Coronavirus Disease 2019 (COVID-19) pandemic, there has been much work to understand the effects on tissues expressing the Angiotensin Converting Enzyme-2 (ACE2) receptor, including the placenta. There is limited information regarding placental pathology findings in mothers with COVID-19 and the effects of COVID-19 on the placenta. The available research reports effects on the fetus ranging from minimal to intrauterine fetal demise.
Objective:
To add to the growing body of literature in the data-sparse zone of COVID-19 and its effects on the placenta and fetus.
Design/Methods: A case report in a high-risk delivery center and level III Neonatal Intensive Care Unit (NICU) in Los Angeles.
Results:
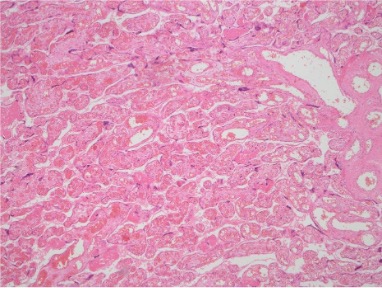
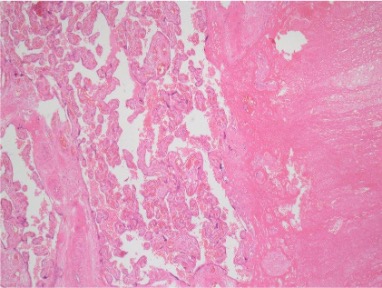
A 4680g baby boy was born at 38+1 weeks of gestation to 36y old G4P1021 female via repeat cesarian section. The pregnancy was complicated by advanced maternal age, chronic hypertension with superimposed pre-eclampsia with severe features, BMI of 80, and COVID-19 infection. The mother had mild COVID symptoms and did not require hospitalization or oxygen support. Prenatal ultrasounds were limited due to body habitus. At delivery, there was clear amniotic fluid. The infant was cyanotic, limp, and was brought to the warmer immediately. Non-invasive positive pressure ventilation started at 5 minutes of life with improvement in color and oxygen saturation. He was then admitted to the NICU. APGARs were 2, 3, 5, and 7 at 1, 5, 10, and 15 minutes respectively. Cord gases showed severe metabolic acidosis. The patient was diagnosed with hypoxic-ischemic encephalopathy (HIE) and therapeutic hypothermia was initiated. The NICU and obstetric teams were unable to identify a clear perinatal cause of HIE. Later, the placental pathology report revealed a large placenta for estimated gestational age corresponding to the 75th percentile, villous parenchyma with focal chorangiosis and thrombi, with unremarkable fetal membrane and three vessel umbilical cord. The cause of HIE was attributed to the placental thrombi likely caused by COVID-19 infection.
Conclusion(s):
Fetal vascular malperfusion and thrombus have been noted as findings in the placentas of pregnant women who test positive for COVID-19. Given the mother’s COVID-19 infection and the placental pathology findings, as well as the lack of clinically evident hypoxic event, it is likely that the cause of this patient’s HIE was due to the effects on the placenta from COVID-19. As more information comes to light about the effects of COVID-19 on the placenta, it is important to consider a COVID-19 infection during pregnancy as a cause of HIE in a newborn.