Gastroenterology/Hepatology
Gastroenterology/Hepatology
57 - Esophageal Fistulization Associated with Chronic Button Battery Exposure in a Pediatric Patient
Publication Number: 57.215

Dina Al-Zubeidi, MD (she/her/hers)
Associate Professor of Pediatrics-Gastroenterology
University of Iowa Stead Family Children's Hospital
Iowa City, Iowa, United States
Brandon T. Brown, MD (he/him/his)
Pediatric GI Fellow
University of Iowa Roy J. and Lucille A. Carver College of Medicine
Iowa City, Iowa, United States
Presenting Author(s)
First Author(s)
Background:
There continues to be an increase in complications and death associated with esophageal button batteries despite AAP and NASPGHAN Advocacy efforts in parent education and ingestion prevention. This continues to be the most critical indication for emergent endoscopy in children. We present a unique case of chronic progressive post prandial vomiting due to button battery ingestion.
Objective: N/A
Design/Methods: N/A
Results:
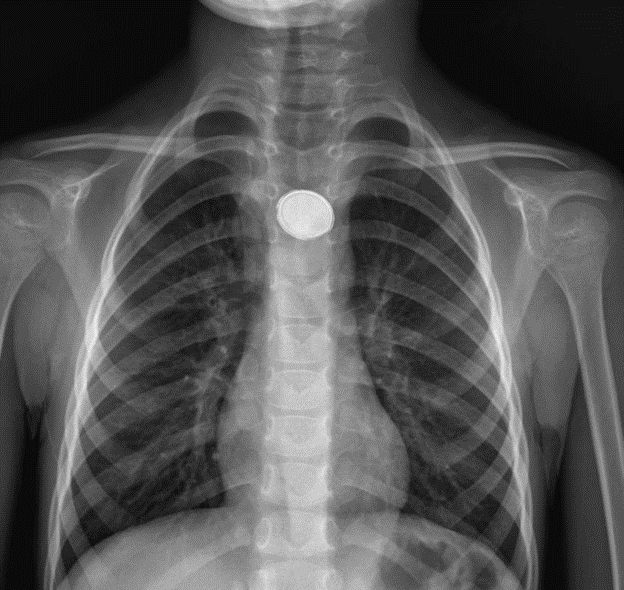
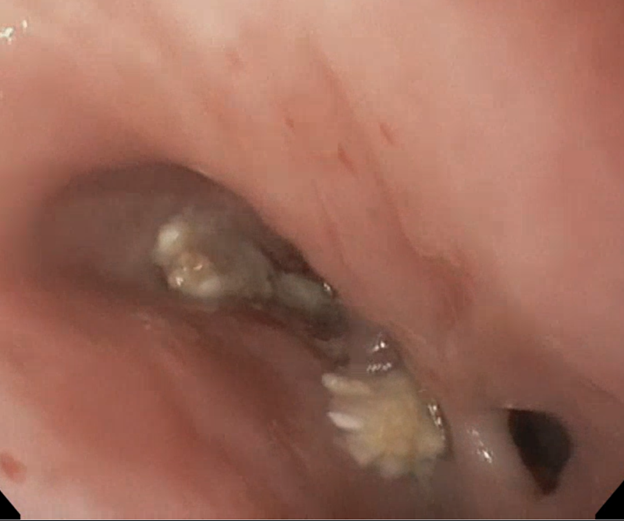
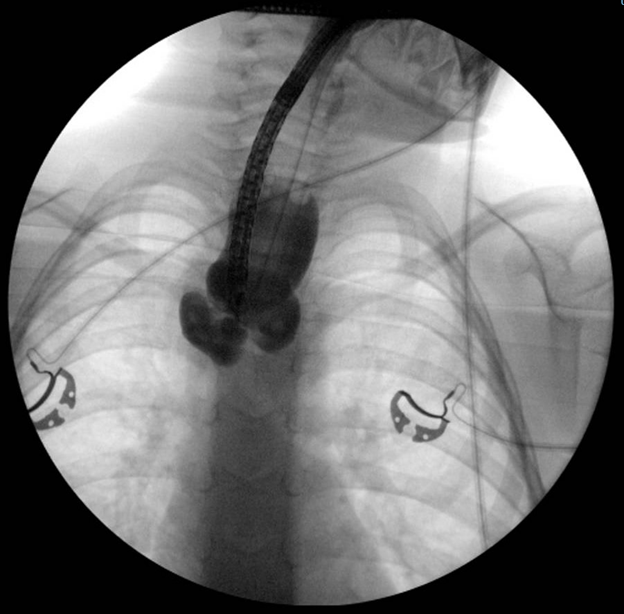
We report a case of a 4-year-old female who presented acutely to the emergency department (ED) with a 1-year history of post prandial vomiting. She had a chronic history of daily non-bloody, non-bilious emesis immediately following feedings. The patient was followed by a pediatric otolaryngologist for management of these symptoms and recently underwent tonsillectomy and adenoidectomy one month prior. Since the procedure, her parents had noted worsening of emesis with feeds, as well as increased nasal drainage, though she continued to gain weight appropriately. Vitals were stable and physical exam was unremarkable. Pediatric Gastroenterology service was consulted, and a chest x-ray was obtained (Figure 1) which showed a 2 cm radiopaque round density in the mid esophagus concerning for a button battery. As the duration of ingestion was unknown, the decision was made to obtain a contrast CT of the chest to evaluate damage to the local structures which showed moderate adjacent esophageal dilatation and wall thickening without signs of perforation. Emergent endoscopic removal of the button battery in the esophagus using rat tooth forceps was done, with multiple fistulous blind-ending tracts identified with no obvious passage to the distal esophagus (Figure 2). There were no signs of acute mucosal injury, erythema or ulceration noted. Laparoscopic placement of a gastrostomy tube followed by esophageal dilation was performed, with elective esophageal reconstructive surgery planned in the future, consisting of resection with primary anastomosis.
Conclusion(s):
Our case highlights the presentation of a child with chronic progression of symptoms associated with prolonged button battery exposure, and not immediately following ingestion. In our case, there were no signs of mucosal injury to indicate an acute process. The chronic duration of her symptoms, and the degree of esophageal fistulizing disease with otherwise healthy appearing mucosa, are likely both related to the initial injury at the time of ingestion, as well as the chronic exposure of the button battery within the esophagus.