Emergency Medicine: All Areas
Emergency Medicine 6
350 - CAUTION: Pediatric Emergency Medicine Suicide Screening may have Predictable Discrepancies that Affect Underserved Populations
Publication Number: 350.21

Steven C. Rogers, MD, MS (he/him/his)
Pediatric Emergency Medicine Physician
Connecticut Children's
Hartford, Connecticut, United States
Presenting Author(s)
Background:
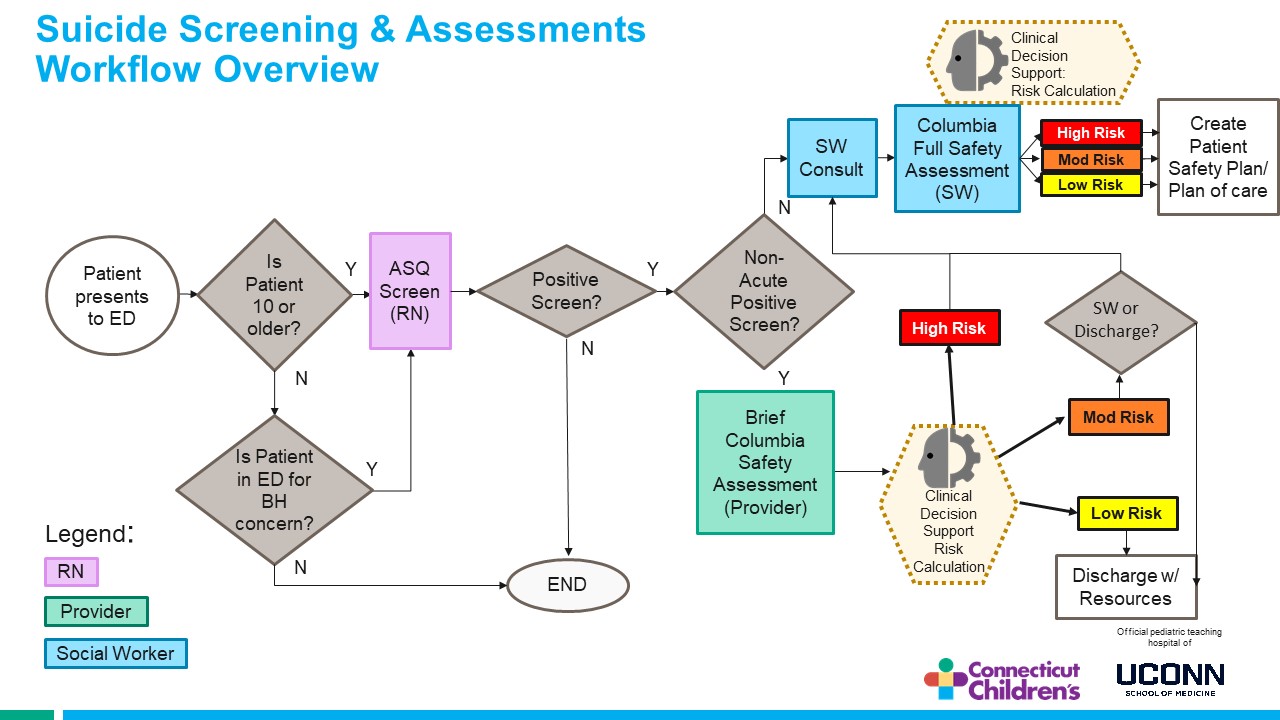
Suicide is a leading cause of death in youth between the ages of 10 and 24 in the United States. The Joint Commission’s National Patient Safety Goal 15.01.01 set standards for suicide prevention in healthcare settings that includes screening, risk assessment and safety planning. Our pediatric emergency department (PED) provides universal screening for all youth 10 years and older with the validated Ask Suicide Questions (ASQ) screening tool. If the screen is positive without acute risk of suicide a confirmatory screen and risk assessment is completed using the brief Columbia Suicide Severity Rating Scale (C-SSRS). The C-SSRS is performed to help providers determine next steps in PED care (see workflow figure).
Objective: Quantify the rates of discrepancy between a non-acute positive ASQ and a low risk C-SSRS response and define any potential predictive characteristics of those individuals.
Design/Methods:
This retrospective chart review study examined youth 10-18 years old presenting to a busy urban PED. Records from 09/2019 – 08/2021 were searched to determine if patient demographics influenced the discrepancies seen between their ASQ and C-SSRS responses for suicide risk. A logistic regression model was created predicting a decrease in suicide risk from being non-acute risk on the ASQ to low risk on the C-SSRS by age, gender, race, and medicaid insurance.
Results:
Over a 2 year-period, 17,366 patients were screened. Of which, 13.7% (n=2380) patients scored non-acute on the ASQ and 71.8% (n=1709) of these patients received a follow-up C-SSRS. Of patients receiving a C-SSRS, 31.1% (n=532) scored low risk on the C-SSRS. Patients being older, identifying as black or Hispanic and having Medicaid insurance (p values < .006) predicted higher risk of a discrepancy between screens. Gender and identifying as another race did not predict discrepancies (p values >.27).
Conclusion(s):
Universal screening for suicide risk in PEDs is a critical opportunity to prevent youth suicide but understanding the limitations of the results is important. Many youth have discrepancies in screening results and those youth have defining predictive characteristics (older, black, Hispanic and Medicaid insured). These underserved youth may require a different screening process and/or response to positive screens. Future studies and quality improvement efforts should focus on improving universal suicide screening for all youth but these underserved populations should be a priority.