Gastroenterology/Hepatology
Gastroenterology/Hepatology
62 - Unintended Consequences and Clinical Outcomes of Proton Pump Inhibitor Therapy in Infants with Varying Levels of Esophageal Acid Exposure
Publication Number: 62.215

Roseanna Helmick, B.S. (she/her/hers)
Senior Research Associate
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background:
Proton pump inhibitor(PPI)s alter gastric acid and therefore esophageal milieu in those with gastroesophageal reflux (GER) or GER disease (GERD). Information is still lacking for use in neonatal ICU (NICU) infants based on the spectrum of objectively determined acid reflux index (ARI).
Objective: Our aim was to evaluate pH-impedance and pharyngo-esophageal motility mechanisms in NICU infants treated with short-term PPI therapy and compare characteristics between those with indeterminate (3-7%) or abnormal ( >7%) ARI.
Design/Methods: NICU infants with ARI >3% (N=36 born at 29.9±4.3 weeks gestation) underwent 4 weeks of PPI with one week of washout. Longitudinal evaluation at weeks 0 and 5 included pH-Impedance testing to assess GER characteristics and symptoms, and provocative pharyngo-esophageal motility to assess the effect of pharyngeal stimuli (sterile water 0.1-0.5 mL) on proximal aero-digestive reflexes. Comparisons were performed using mixed models between infants with indeterminate (3-7%) and abnormal ( >7%) ARI for clinical outcomes (growth, feeding and breathing methods, length of hospital stay, neurodevelopment), pH-impedance metrics (acid reflux index, distal baseline impedance, number of GER events, bolus clearance time, symptoms), and sensory-motor pharyngo-esophageal motility characteristics (response latency, magnitude, and duration).
Results:
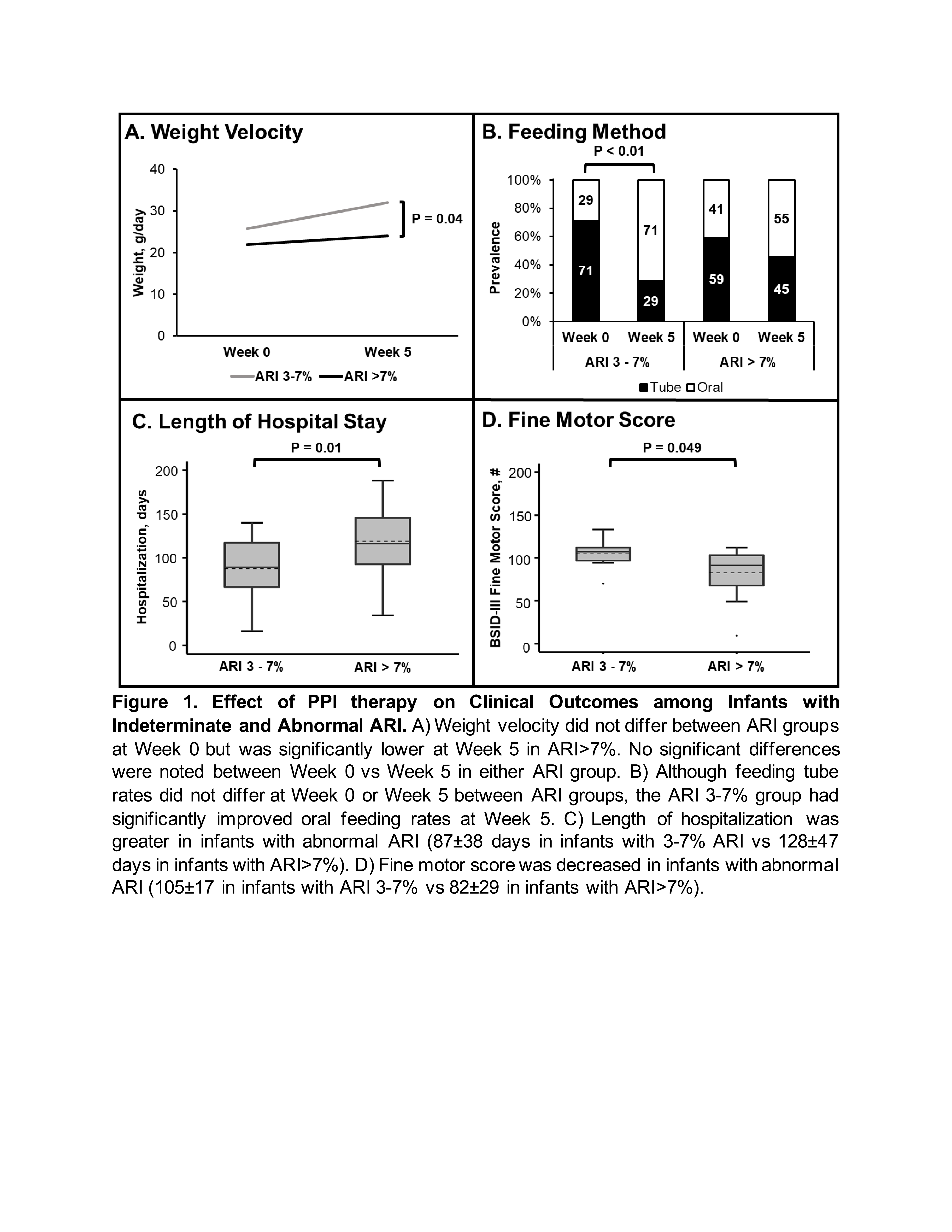
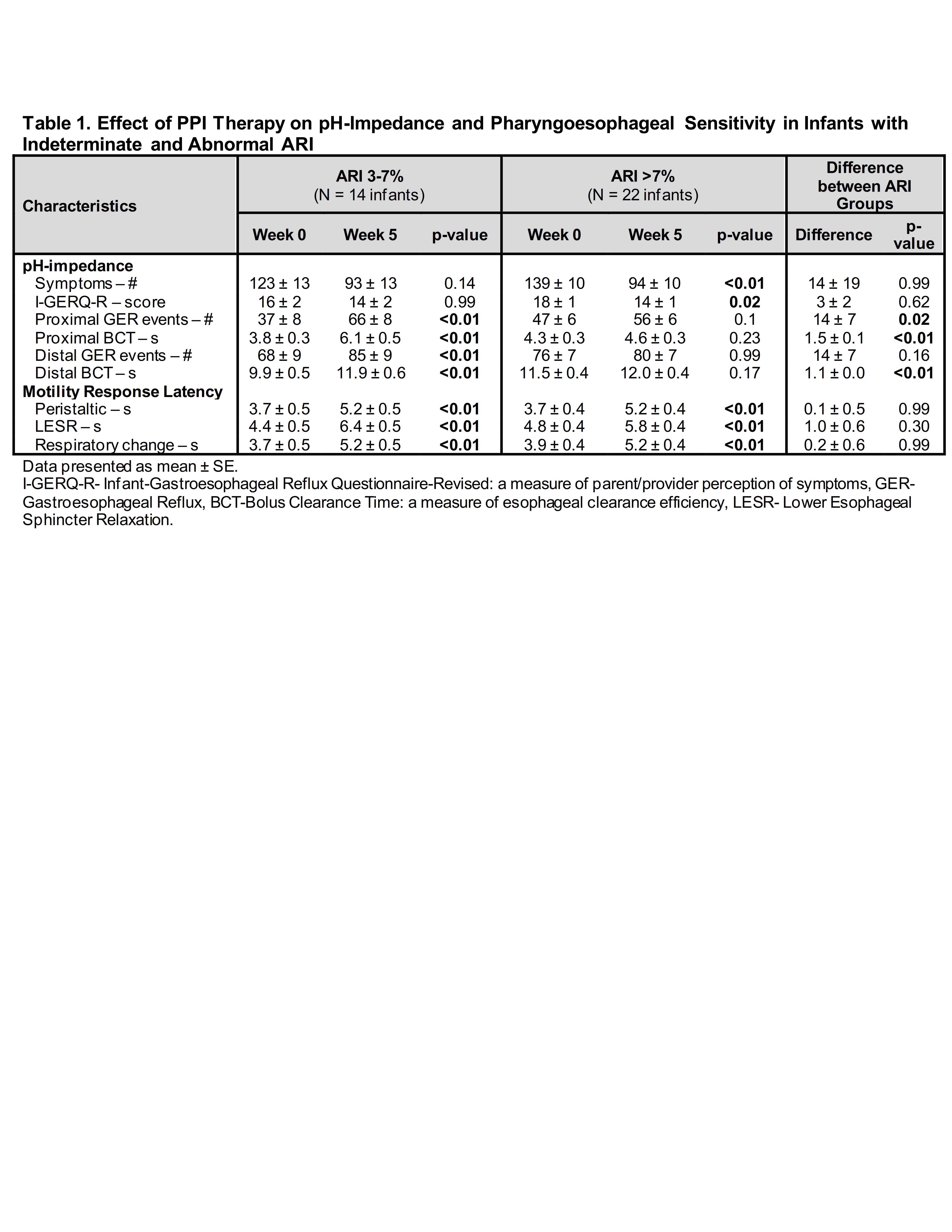
After completion of 4 weeks of PPI treatment, infants with ARI >7% had worse clinical outcomes compared to those with ARI 3-7% (details in Figure 1), but lesser frequency of symptoms and parent/provider perception of symptoms (Table 1). Infants with ARI 3-7% treated with PPI had increase in number of proximal and distal GER events, and prolonged proximal and bolus clearance with no change in symptoms (Table 1). Additionally, response sensitivities decreased after PPI regardless of ARI severity, as evidenced by increased response latencies for peristaltic, lower esophageal, and respiratory responses at Week 5 for both ARI groups (Table 1).
Conclusion(s):
PPI therapy in infants treated for GERD likely has short-term and long-term consequences. Empiric treatment for GERD without any evidence may amplify the risk of consequences. Distinct differences exist in mechanistic characteristics after PPI therapy, as well as between ARI severities. It is unknown if results are due to PPI, GERD pathophysiology, or other co-morbidities. Careful patient selection strategies for defined therapies and further controlled studies with placebo are needed.