Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 2: Physiology 1
340 - Use Of Lung Ultrasound Versus Radiography In Neonates With Transient Tachypnea Of The Newborn
Publication Number: 340.345

Maria Brandani, Md (she/her/hers)
Neonatologist
Hospital Italiano de Buenos Aires
CABA, Buenos Aires, Argentina
Presenting Author(s)
Background:
Transient tachypnea of the newborn (TTN) is the clinical manifestation of delayed fetal lung fluid clearance. Usually improves within 24-48 h and chest X-ray shows a pattern known as "wet lung". Treatment varies from titrated oxygen hood to CPAP. Diagnosis is retrospective and diagnostic findings are nonspecific. Lung ultrasound (LU) is an accurate, bedside, reproducible and non-invasive diagnostic tool which allows to evaluate the gradual transition from a wet to an air-filled lung. LU may be useful to decide the discontinuation of supportive measures.
Objective: 1)To compare the time of respiratory support from first hours of life to their withdrawal, between two groups: Group 1: assessed by chest X-ray only vs Group 2: assessed with LU and chest X-ray. 2)To compare the time (hours) of NICU stay, and the type of respiratory support between groups.
Design/Methods: Retrospective study including all inborn 34.0-40.6 wk GA admitted to NICU with TTN who required oxygen hood or CPAP between Jan 2020 to Dec 2021. Exclusion criteria: use of mechanical ventilation, surfactant, congenital malformations, sepsis, chorioamnionitis and pneumothorax. LU was performed once, within 12 hours of life, during respiratory support. Baseline characteristics and main outcomes were compared between groups.
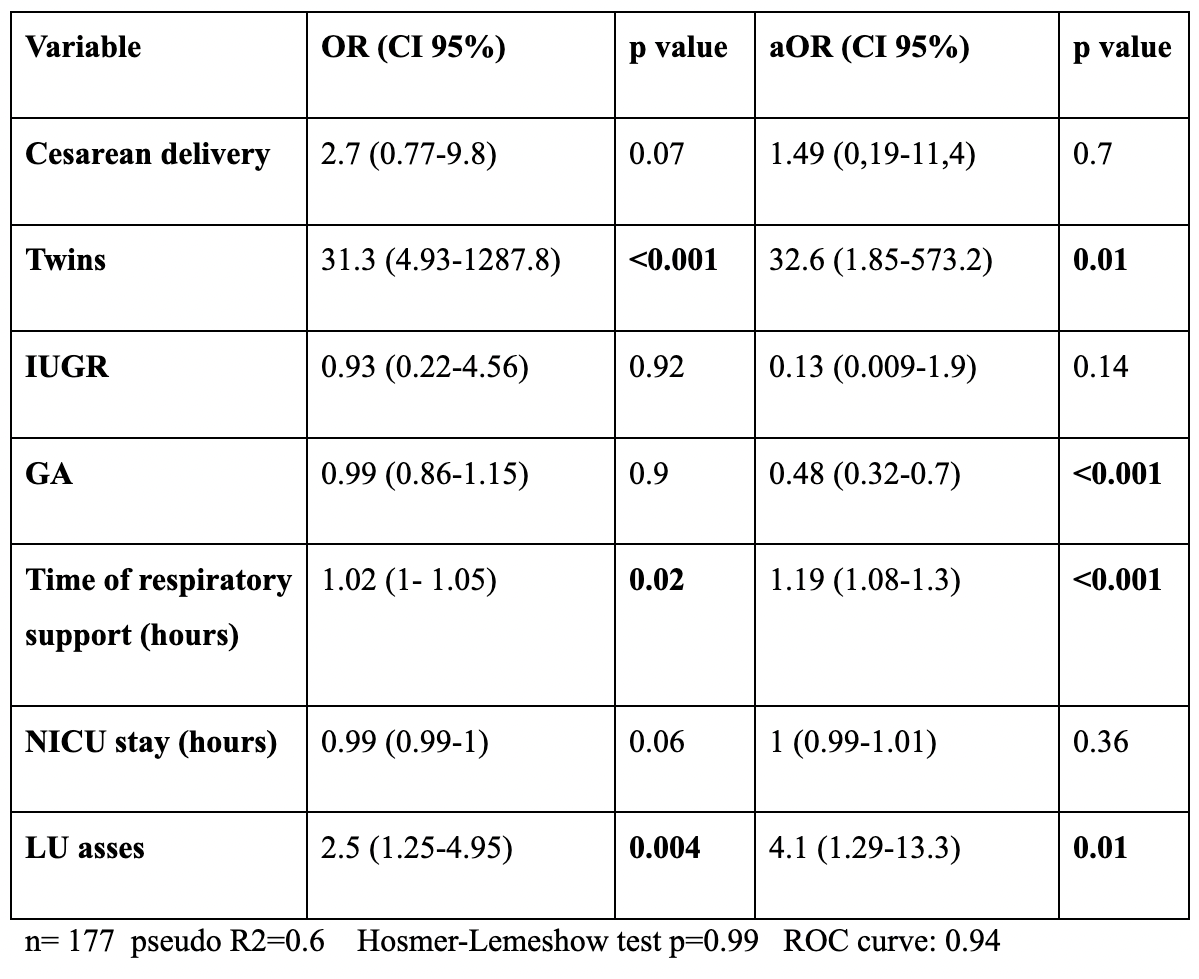
Time-related outcomes were also analyzed with Kaplan Meier curves. Stratified analysis by GA and type of respiratory support was performed. To identify independent variables associated with CPAP, univariate and multivariate analysis were performed. P value < 0.05 was statistically significant. Stata version 13 and R Studio were used for data analysis. This study was approved by the local Ethics Committee.
Results: 177 patients were included, 69 in group 1 and 108 in group 2 (61%). Baseline characteristics were similar between groups except IUGR (13% vs 2% p=0,004) and meconium-stained amniotic fluid (10,3 vs 0,9% p=0,006). A statistically significant difference was observed in time of respiratory support (p=0.001) and no difference regarding NICU stay between groups (p=0.64). In multivariate analysis, LU assessment was 4.1 fold (CI 95%: 1.29-13.3) associated with CPAP use, adjusted by cesarean section, twins, IUGR, GA, time of respiratory support and NICU stay.
Conclusion(s): Patients assessed by LU and chest X-ray had longer respiratory support time compared to the other group, in late preterms, but not in term babies. Despite this finding, there were no differences in NICU stay between groups. The use of LU was independently associated with CPAP use.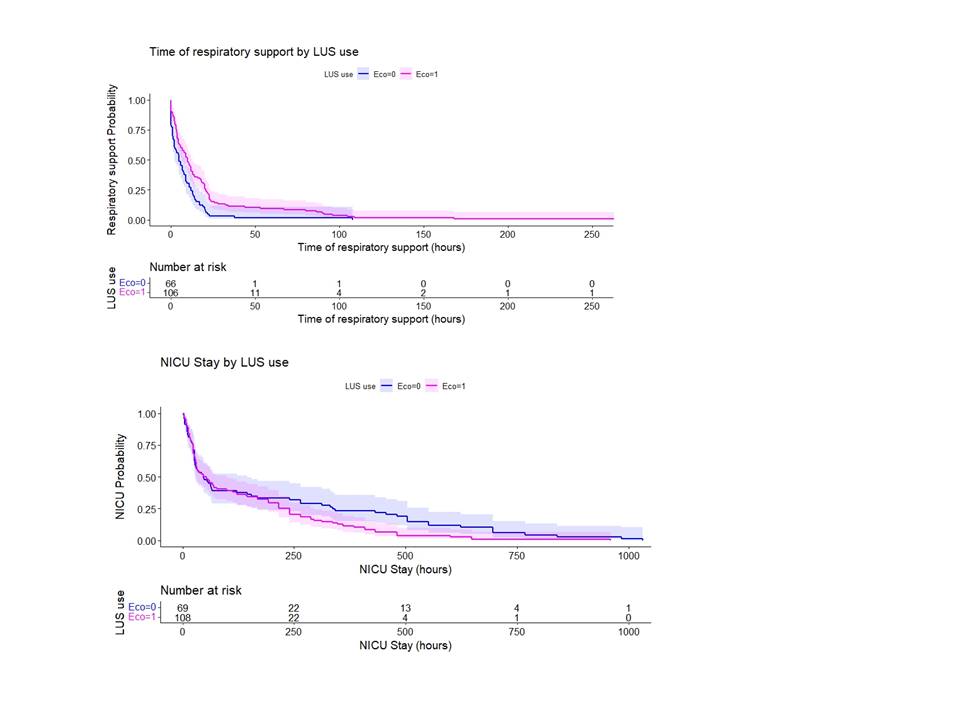
.png)