Neonatal General
Neonatal General 7: NICU Practices 1
179 - Utility and Timing of Screening Head Ultrasounds in Preterm Neonates
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 179
Publication Number: 179.331
Publication Number: 179.331
Hadi Berbari, Creighton University School of Medicine, phoenix, AZ, United States; Victoria Johnson, Creighton University School of Medicine, Omaha, NE, United States; Sarah Batt, Creighton University School of Medicine, Phoenix, AZ, United States; Soumini Chintala, Phoenix Children's Hospital, Phoenix, AZ, United States; Mohammad Bader, University of Arizona, Phoenix, AZ, United States; Hemananda K. Muniraman, Phoenix Children's Hospital, PHOENIX, AZ, United States

Hadi Berbari, BS (he/him/his)
Medical Student
Creighton University School of Medicine
phoenix, Arizona, United States
Presenting Author(s)
Background: In 2020, The American Academy of Pediatrics (AAP) published clinical report on routine neuroimaging in preterm infants recommending routine head ultrasound (HUS) at 7-10 days of life (HUS1), 4 to 6 weeks of age (HUS2), and at either term equivalent (TEA) age or near discharge (HUS3). The initial screening head ultrasound is critical since most intraventricular hemorrhages (IVH) occur during the first week of life.
Objective: Our objective was to determine the utility of follow-up HUSs following a normal first HUS.
Design/Methods: Retrospective cohort study including preterm infants born below 32 weeks and birth weight of 1500 grams in a level III neonatal intensive care unit between Jan 2016-Dec 2022. Timing and abnormalities reported on HUS were described in infants. Infants' characteristics, birth history, and neonatal course were reviewed and described for infants with a normal first HUS and abnormal follow-up abnormal HUS.
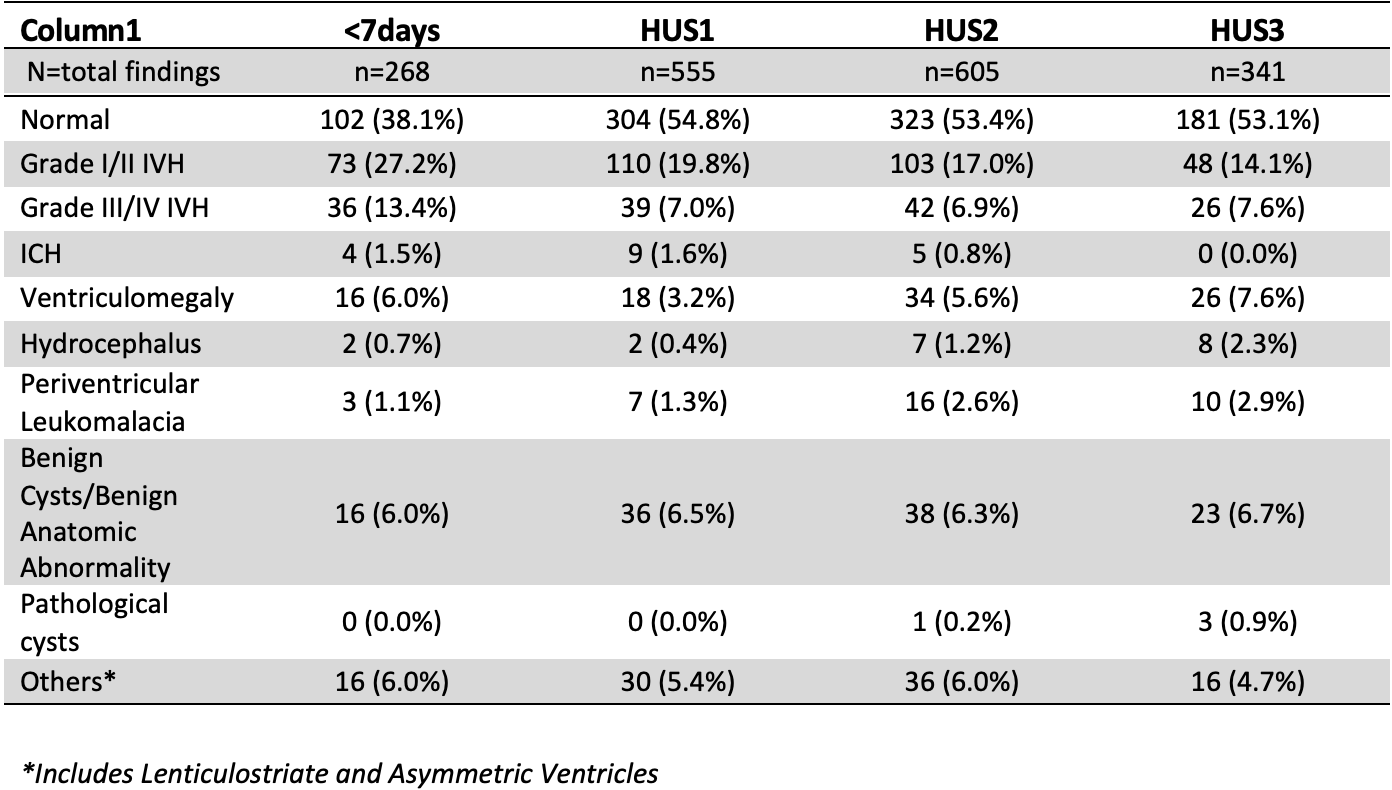
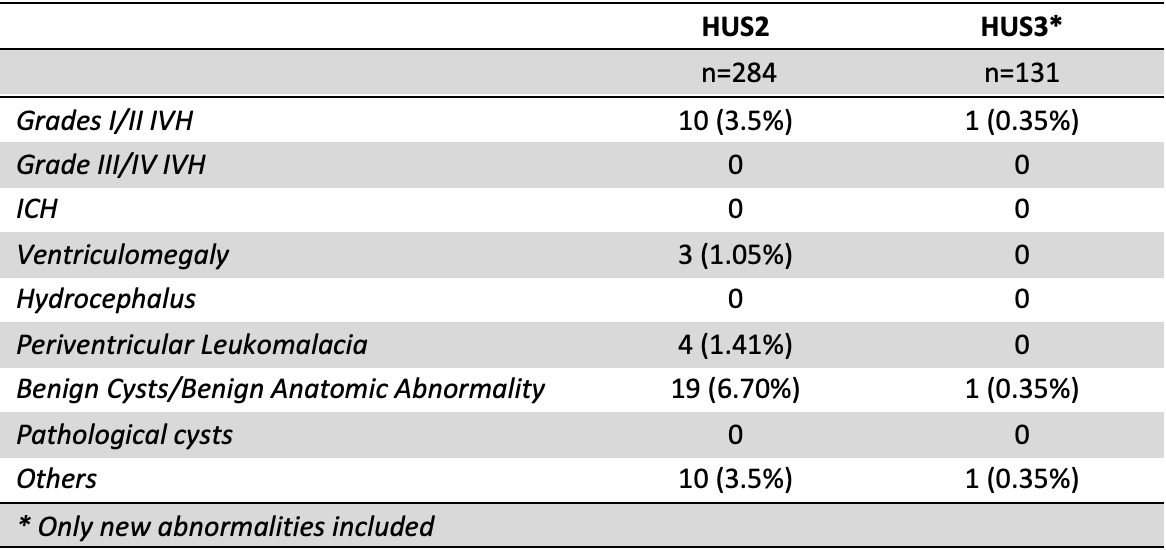
Results: A total of 577 patients were included of which, 215 (37.3%) had their initial HUS performed before the 7th day of life. In this subset, HUS was reported as normal, grade I/II IVH, and grade III/IV in 102 (38.1%), 73 (27.2%), and 36(13.4%) infants respectively. 485 neonates underwent HUS1 of which, 304 (54.8%) were normal, 110(19.8%) revealed grade I/II IVH, and 39 (7.0%) grade III/IV IVH (Table I). 508 neonates underwent HUS2 of which 284 infants were following a normal HUS1. 43 (14.1%) were identified to have new abnormalities on HUS2. The most common new findings were benign cysts/benign anatomic abnormalities (6.7% of scans), followed by Grade I/II IVH at 3.5% with no severe IVH detected. Twenty-four patients had a resolution of findings between HUS2 and HUS3 (Table II). 341 infants had HUS3, 131 following a normal HUS1 with three patients were found to have new abnormalities (grade I IVH, choroid plexus cyst, and echogenicity in the right cerebellar fossa) (Table II).
Conclusion(s): We report that in infants with a normal first HUS, one in eight (14.1%) and one in 43 (2.3%) infants had new abnormalities detected on HUS2, and HUS3, the majority of these new abnormalities were benign or self-limiting. In an otherwise uncomplicated neonatal course and an unremarkable initial HUS1, a single HUS performed at either 4-6 weeks or TEA may be sufficient to detect all subsequent consequential abnormalities and may lead to better resource utilization. However larger studies are required to make conclusive recommendations.