Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 3: Physiology 2 and Clinical Outcomes
353 - Oxygen Saturation (SpO2) Stability after Initiation of Sedation in Preterm Infants on Invasive Mechanical Ventilation
Publication Number: 353.346
- ML
Mei Mei Lam (she/her/hers)
Fellow
BC Women's Hospital
Richmond, British Columbia, Canada
Presenting Author(s)
Background:
The use of sedation to improve respiratory stability in preterm infants on invasive mechanical ventilation (IMV) has not been recommended despite being commonly used in Neonatal Intensive Care Units. The effect of initiating sedation on respiratory stability remains unknown. SpO2 histogram quantifies SpO2 distribution and can be used as an indicator of respiratory stability.
Objective:
To determine the effect of sedation on improving respiratory stability in preterm infants requiring IMV, as characterized by SpO2 histogram in the first 24 hours after initiation of sedation.
Design/Methods:
A retrospective review was conducted on preterm infants born < 37 weeks gestational age who were started on sedation for the first time while requiring IMV between January 2019 and November 2020. We excluded infants receiving postoperative or post-procedure sedation or on therapeutic hypothermia, and those with previous sedation exposure. Clinical characteristics, SpO2 histograms, ventilation settings and oxygen requirements within 24 hours from sedation starting were reviewed.
Results:
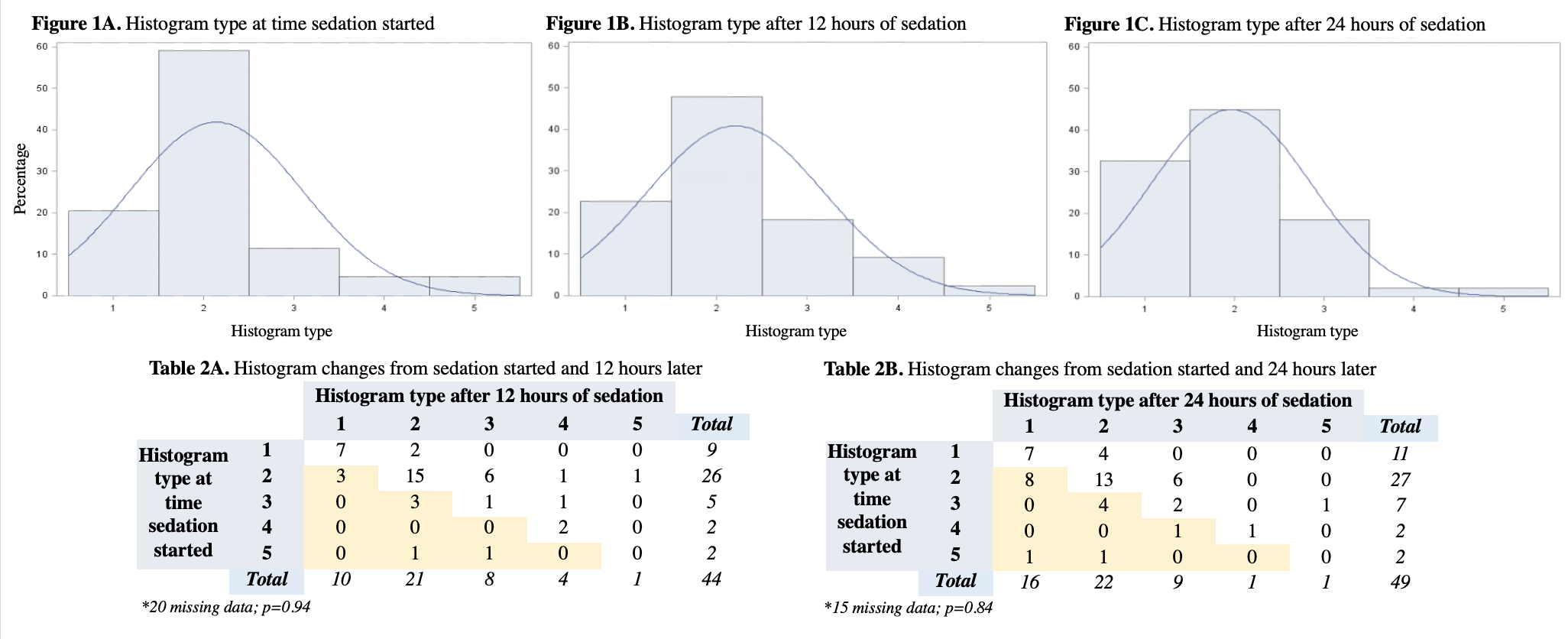
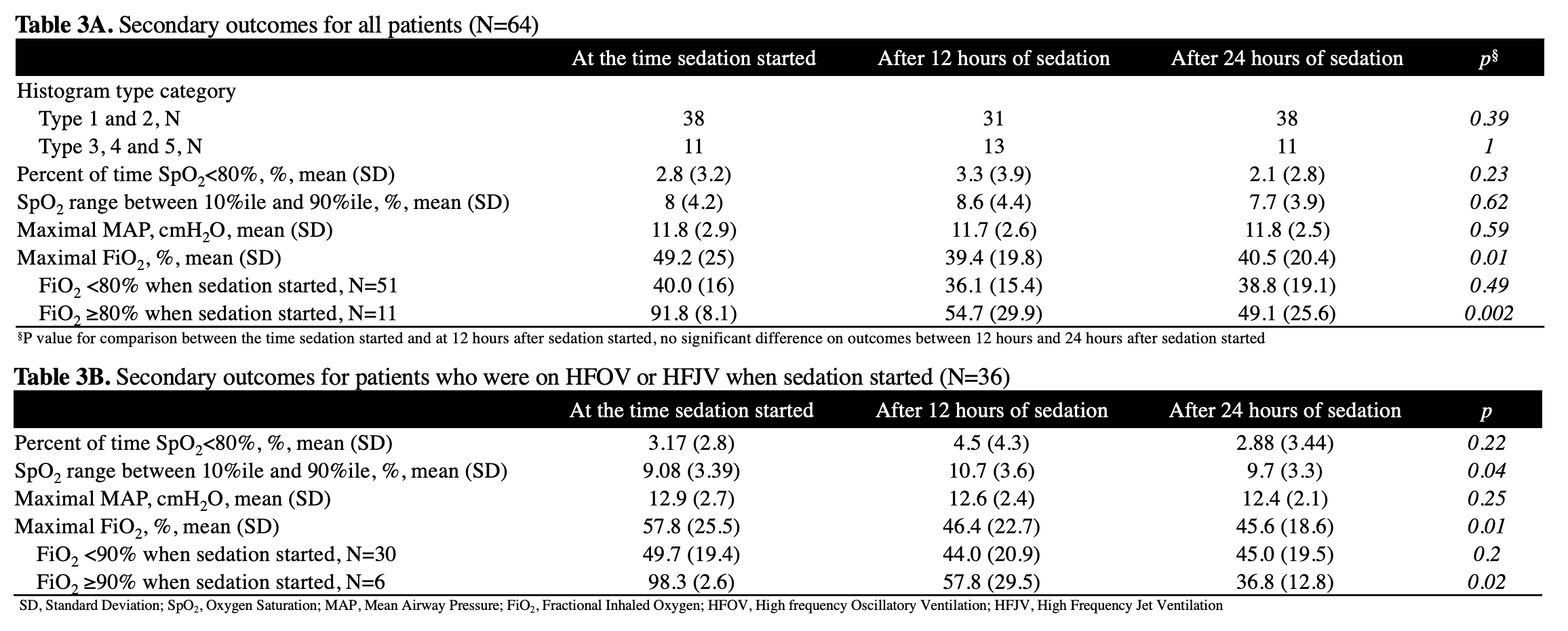
A total of 64 preterm infants (42 females) were included. 35 (55%) infants were started on morphine and 29 (45%) were started on fentanyl. 60 (94%) infants were started on a continuous infusion at a median rate of 10mg/kg/hr of morphine or 1mcg/kg/hr of fentanyl. The median cumulative dose in the first 24 hours was 290mg/kg of morphine or 26 mcg/kg of fentanyl (Table 1). By examining SpO2 histograms within the first 24 hours of sedation initiation, we found that 80% (35/44) of infants had SpO2 histograms of type 1 and 2 when sedation started, indicating a stable respiratory status. The SpO2 histogram types were not significantly different from sedation starting and 12 hours (P=0.93) and 24 hours later (P=0.84) (Table 2 and Figure 1). No significant difference on percent of time SpO2 was < 80% (2.8% vs. 3.3%, P=0.23), range of SpO2 between 10%ile and 90%ile (8% vs. 8.6%, P=0.62) and the maximal mean airway pressure (11.8 vs. 11.7, P=0.59) from sedation starting and 12 hours later. The maximum fractional inhaled oxygen (FiO2) was significantly lower 12 hours after sedation started (49.2% vs. 39.4%, P=0.01). However, when the FiO2 was less than 80% when sedation started, the significant difference no longer stood (40.0% vs. 36.1%, P=0.49) (Table 3).
Conclusion(s):
In preterm infants requiring IMV, initiating sedation did not significantly improve respiratory stability as characterized by SpO2 histogram. Providing sedation may reduce FiO2 requirement in infants with highest pre-sedation FiO2 needs. .png)