Neonatal Neurology: Clinical Research
Neonatal Neurology 6: Clinical 6
133 - Cerebral tissue oxygenation in the first week among preterm neonates is associated with the General Movements Assessment
Publication Number: 133.338
.jpg)
Amy Rothwell (she/her/hers)
Medical Student
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background:
Preterm infants are at high risk for brain injury, which can lead to a diagnosis of cerebral palsy (CP) in childhood. The general movements assessment (GMA) is a validated screening tool with high predictability of CP used to evaluate former preterm infants prior to neonatal intensive care unit (NICU) discharge. Monitoring cerebral tissue oxygenation (CrSO2) with near-infrared spectroscopy (NIRS) is increasingly used in the NICU to detect cerebral hypoxia and potentially reduce the risk of future neurodevelopmental abnormalities like CP. No prior studies among preterm infants have evaluated the relationship between CrSO2 values and the GMA.
Objective: To determine the relationship between CrSO2 and GMA among preterm infants at NICU discharge.
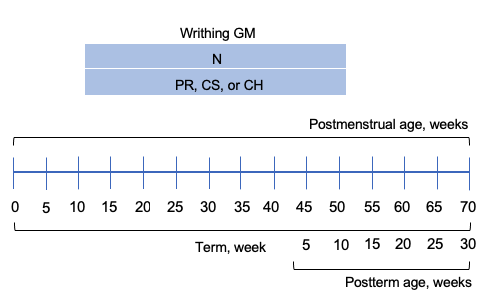
Design/Methods: A secondary retrospective analysis of a prospective NIRS study was performed. INVOS NIRS sensors were placed on neonates < 32 weeks within 48 hours of age. Continuous, every 5-second CrSO2 data was collected until 7 days of age. Means were calculated in 12-hour epochs from 48 hours to 168 hours of age. GMA results, classified as normal (writhing) or abnormal (poor repertoire) (Figure 1), and head ultrasound (HUS) findings identified prior to NICU discharge were included. Abnormal HUS was defined as any-grade intraventricular hemorrhage or periventricular leukomalacia.
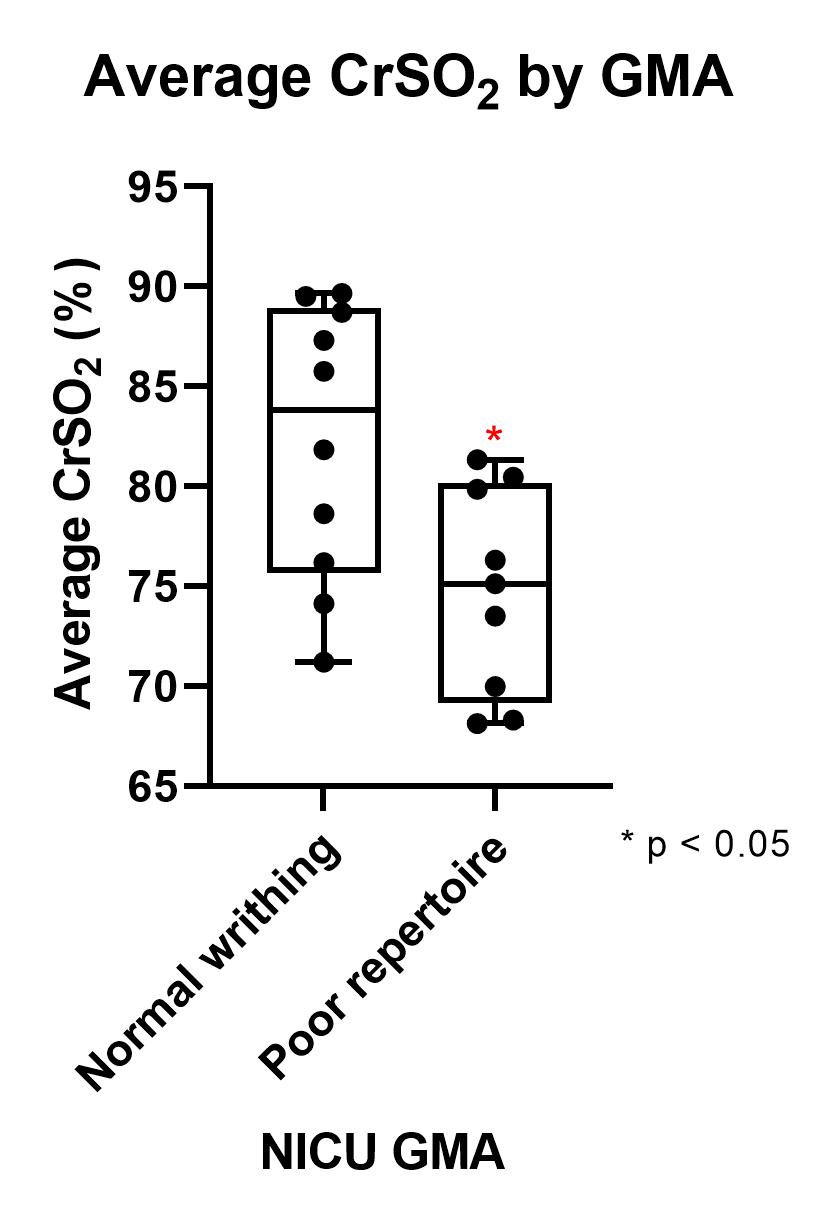
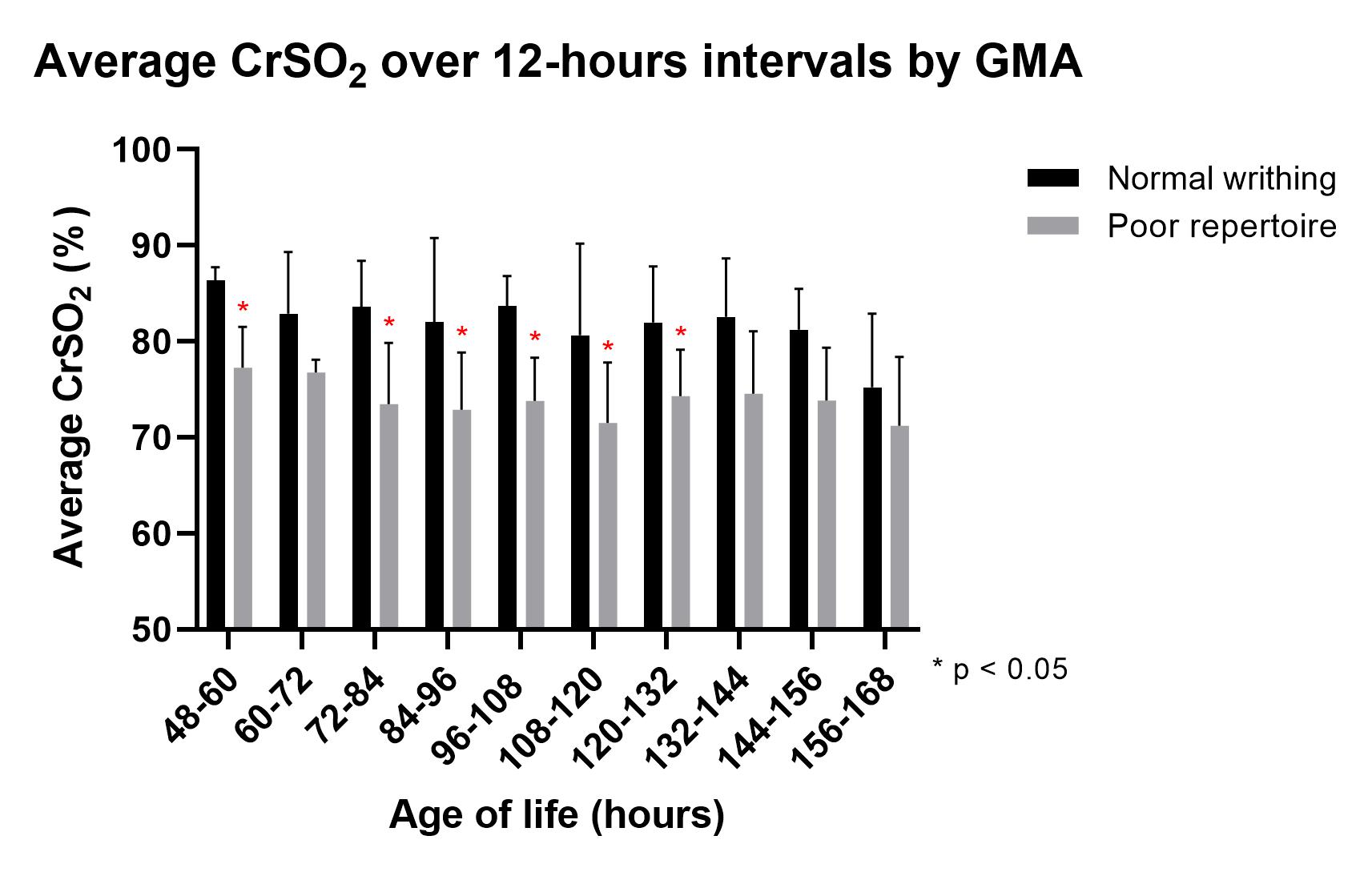
Results: GMA was performed prior to NICU discharge for 19 of 35 neonates, with mean gestational age of 29.2 ± 2.4 weeks and mean birth weight of 1315 ± 399 g. Mean time of GMA was 35.7 ± 1.2 weeks post menstrual age, with 10 scoring normal writhing and 9 with poor repertoire. Average continuous CrSO2 was significantly lower in infants demonstrating poor repertoire on GMA compared to those with normal writhing (75.14 vs. 83.81, p< 0.05, Figure 2). This significance was appreciated in 12-hour intervals starting at 48, 72, 84, 96, 108, and 120 hours (Figure 3). HUS showed abnormalities in 0.0% with normal writhing and 33.3% with poor repertoire. No significant differences in CrSO2 were seen when GMA subgroups were further divided by HUS results.
Conclusion(s):
In this pilot study, preterm infants with poor repertoire on GMA demonstrated significantly lower CrSO2 values in the first week of age, specifically from 48 to 132 hours. This preliminary analysis suggests that CrSO2 values in the first week may be used as a surrogate measure for future CP diagnoses. Further investigation is needed to characterize differences in CrSO2 associated with GMA in preterm infants, and to evaluate the relationship between early cerebral oxygenation, GMA, and long-term neurodevelopmental outcomes.