Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 1: Lung US - BPD
296 - Non-invasive Ventilation to Prevent Tracheostomy among Neonates with Severe Bronchopulmonary Dysplasia
Publication Number: 296.344
Mark F. Weems, MD
Associate Professor of Pediatrics
University of Tennessee Health Science Center
Memphis, Tennessee, United States
Presenting Author(s)
Background:
Premature infants with severe bronchopulmonary dysplasia (sBPD) may be offered tracheostomy to support long-term mechanical ventilation. While there are no standard criteria in this population, most centers will support patients with continuous positive airway pressure or nasal cannula and proceed with tracheostomy for infants who cannot be extubated by 44 weeks postmenstrual age. A recent shortage of home nursing has led our center to seek innovative methods to support sBPD patients without tracheostomy.
Objective:
We aim to describe a novel strategy of non-synchronized non-invasive positive pressure ventilation (NIPPV) used to support patients with sBPD without tracheostomy in a single Level IV NICU.
Design/Methods:
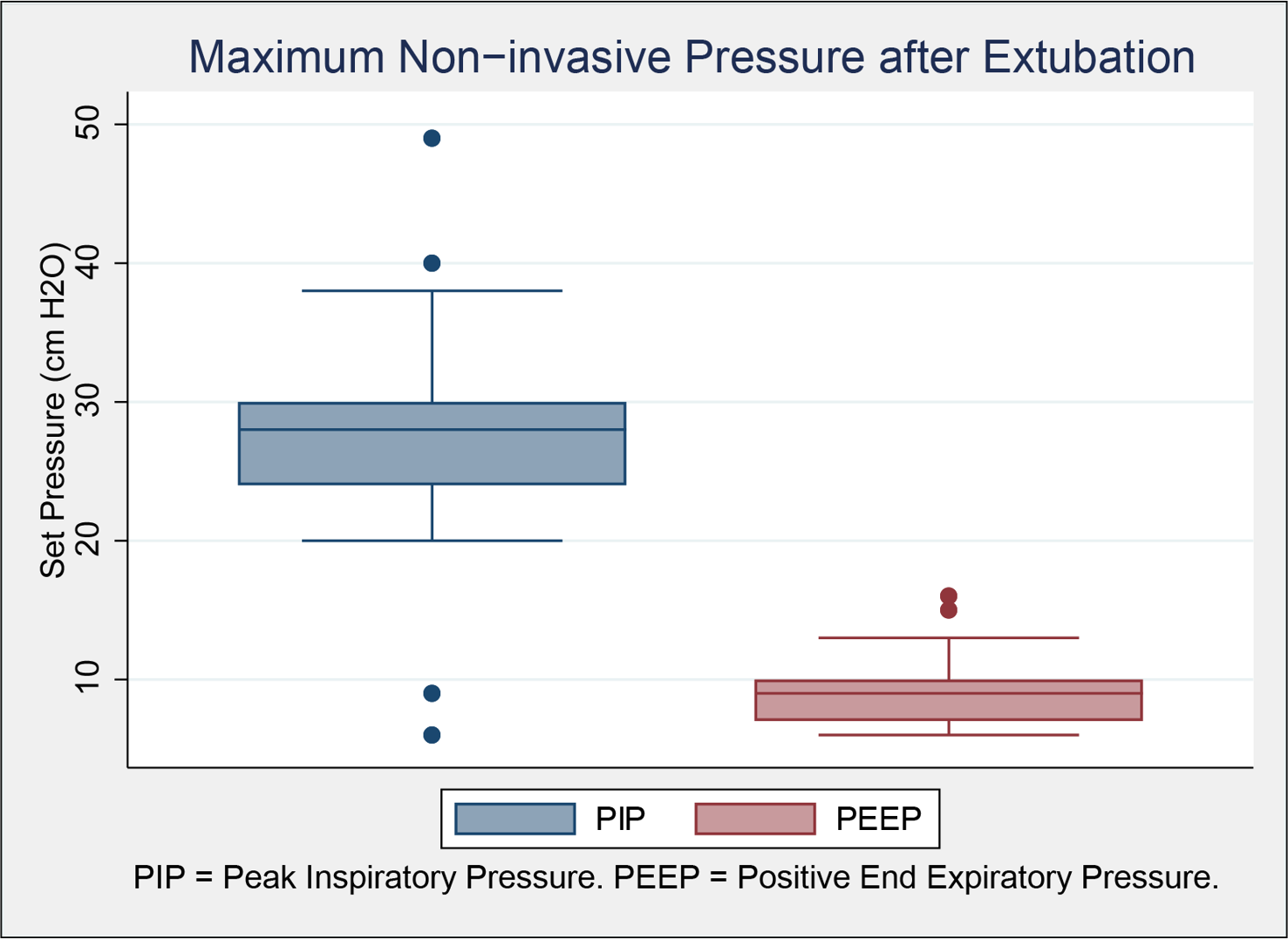
Patients were included in this retrospective study if they were born prior to 32 weeks’ gestation, remained on positive pressure ventilation at 36 weeks postmenstrual age (PMA), and were discharged from January 2020 to December 2022. Patients were divided into tracheostomy and NIPPV groups. The respiratory severity score (RSS) was defined as the product of the FiO2 and mean airway pressure, calculated at 36 weeks PMA and on the calendar day prior to tracheostomy or successful extubation. NIPPV was delivered via the RAM Cannula® using a rate of 40 and inspiratory time 0.5 seconds. PIP and PEEP were set higher than invasive settings, and PIP was weaned before rate or PEEP.
Results:
52 patients were included; 15 were treated with tracheostomy and 37 were successfully extubated without tracheostomy. Demographics and outcomes are shown in Table 1. Results for those patients who remained intubated at 36 weeks PMA are shown in Table 2. RSS at 36 weeks PMA was equal between groups but changed over time. RSS on the day prior to tracheostomy was higher than on the day prior to successful extubation. Tracheostomy placement was associated with an increased length of hospital stay compared to NIPPV. Among the tracheostomy group, 11 had an airway anomaly, 11 were discharged on mechanical ventilation, 2 were discharged with a tracheostomy collar, and 2 remain hospitalized after transfer to another unit. 26 NIPPV patients were discharged with supplemental oxygen, and 11 were discharged without respiratory support. Maximum NIPPV peak inspiratory pressure and end expiratory pressure are shown in the figure.
Conclusion(s): We show a subset of sBPD patients can successfully be extubated from mechanical ventilation using a novel NIPPV strategy without tracheostomy. This strategy may be associated with decreased tracheostomy and length of hospital stay.
.png)
.png)
