Neonatal General
Neonatal General 9: NOWS and Other Exposures
206 - Predictors of Pharmacologic Treatment in Neonates with Prenatal Opioid Exposure
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 206
Publication Number: 206.333
Publication Number: 206.333
Megan Chang, LAC+USC/USC Keck School of Medicine, Los Angeles, CA, United States; Lorayne Barton, LAC+USC Medical Center, Los Angeles, CA, United States; Smeeta R. Sardesai, Keck School of Medicine of the University of Southern California, Arcadia, CA, United States; Rangasamy Ramanathan, Keck School of Medicine of USC, Los Angeles, CA, United States; Rowena Cayabyab, University of Southern California/LAC+USC Medical Center, Los Angeles, CA, United States

Megan Chang, MD (she/her/hers)
Neonatology Fellow
LAC+USC/USC Keck School of Medicine
Los Angeles, California, United States
Presenting Author(s)
Background: Incidence of Neonatal Opioid Withdrawal Syndrome (NOWS) continues to rise. Less is known about characteristics that predispose opioid-exposed infants to pharmacologic intervention.
Objective: Our objective was to characterize our institution’s pharmacologic approach to NOWS and evaluate predictors for pharmacotherapy.
Design/Methods: We performed a retrospective chart review of neonates with prenatal opioid exposure admitted to an urban Level III neonatal intensive care unit (NICU) between 1/2017–2/2022. Prenatal opioid exposure was identified by maternal or neonatal urine toxicology positive for opiates and/or maternal self-reported opiate use during pregnancy. We collected data to evaluate maternal characteristics, neonatal outcomes, and pharmacologic treatment for opiate-exposed infants.
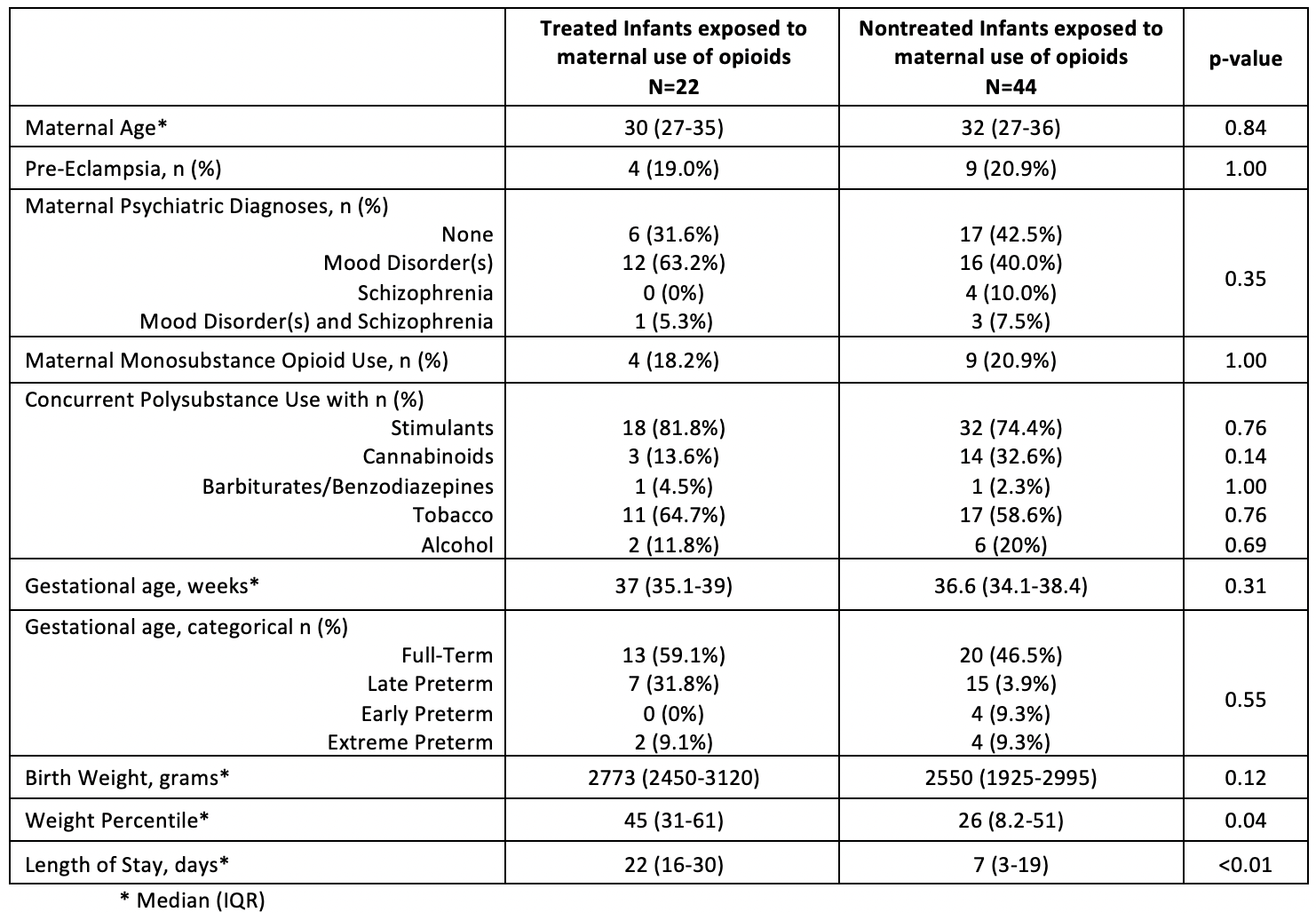
Results: We identified 66 opioid-exposed neonates, with 22/66 (33%) receiving pharmacotherapy with morphine 20/22 (91%) or methadone 2/22 (9%). Infants requiring pharmacotherapy received a median oral morphine dose of 0.073 mg/kg every three hours. Treated infants had a median of 71 morphine doses throughout admission, with median treatment duration of 15 days. In treated infants, maternal isolated mood disorder and concurrent stimulant use were the most common maternal psychiatric diagnosis and type of polysubstance use. However, maternal psychiatric history, concurrent polysubstance use, age, race, and medical comorbidities were not significantly different between non-treated and treated infants. The two cohorts also had no significant differences in gestational age and birth weight. Infants receiving pharmacotherapy had higher weight percentiles and longer lengths of stay (LOS) (Table).
Conclusion(s): Maternal factors such as medical/psychiatric comorbidities and additional substance use did not increase the incidence of pharmacologic management. Appropriately grown infants were more likely to be treated for NOWS. Implementation of Eat, Sleep, Console (ESC) has been started in our NICU and we plan to assess the impact of initiating ESC on LOS and duration of pharmacotherapy.