Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 3: Physiology 2 and Clinical Outcomes
352 - Respiratory severity score as a predictive factor for need for surfactant administration
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 352
Publication Number: 352.346
Publication Number: 352.346
Jack Koueik, American Family Children's Hospital, Madison, WI, United States; Henry Zapata, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Heather L. Becker, Madison College, Waunakee, WI, United States; Michael R. Lasarev, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Dinushan C. Kaluarachchi, University of Wisconsin - Madison, Madison, WI, United States
- JK
Jack Koueik, MD
Pediatrics Resident
American Family Children's Hospital
Madison, Wisconsin, United States
Presenting Author(s)
Background: Preterm infants are at high risk of respiratory distress syndrome (RDS) due to surfactant deficiency. Current clinical management guiding exogenous surfactant replacement is based on need for higher fraction of oxygen to maintain target oxygen saturation. This approach leads to delay in timely administration of surfactant. Also, using only FiO2 as the sole criteria can be misleading. In this study, we aim to evaluate the role of respiratory severity score (RSS) as an early predictive factor for need for surfactant administration in preterm infants.
Objective: To evaluate the role of RSS during the first 2 hours of life as a predictive factor for need for surfactant administration within first 72 hours of life in moderate preterm infant.
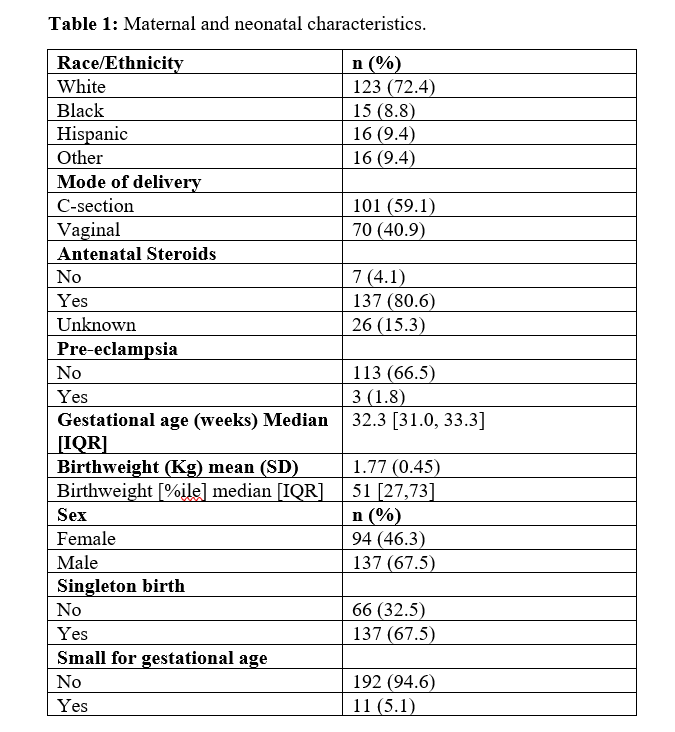
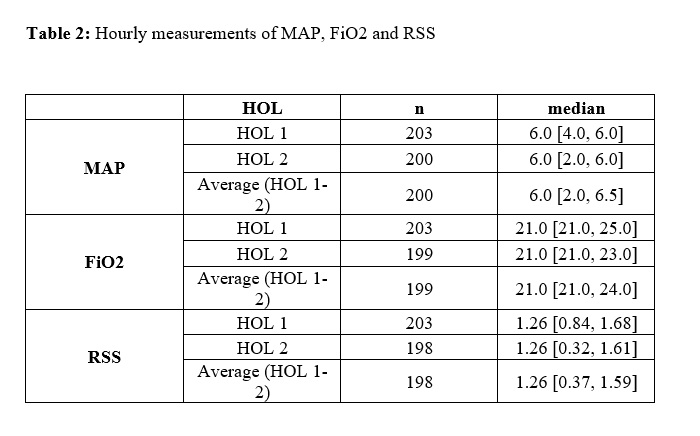
Design/Methods: We conducted a retrospective cohort study of preterm infants born at 28 0/7 to 33 6/7 weeks gestation. Hourly mean airway pressure and FiO2 were collected during the first 2 hours which were used to calculate the RSS (MAP x FiO2). Exclusion criteria included intubation, mechanical ventilation or surfactant administration prior to 2 hours of life as well as major congenital anomalies. A Log-binomial regression model was used to evaluate the association between RSS and need for surfactant administration.
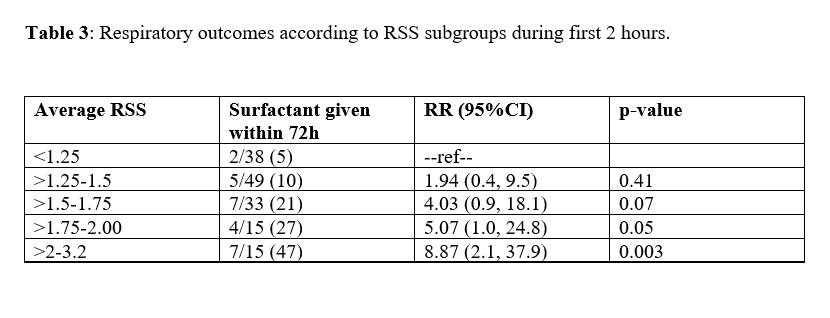
Results: Of 203 neonates, median gestation age was 32.3 weeks with average weight 1.77 kg (table 1). 68% of neonates were on CPAP. Median RSS was 1.26 at 1 and 2 hours of life (table 2). 27 neonates (13.3%) received exogenous surfactant. 48 neonates had average RSS = 0 indicating they remained on room air and were not included in the remainder of the analysis. Risk of needing surfactant administration during the first 72 hours was associated with average RSS score (p = 0.002). Risk for surfactant administration within the first 72 hours increased by 2.06-fold for each 0.5-unit increase in average RSS (RR=2.06; 95% CI: 1.56–2.70, p < 0.001). Average RSS for the first 2 hours was divided into five non-overlapping intervals with a length of 0.25 units. The risk ratios associated with receiving surfactant within 72hours are found to increase with increasing level of the group (Table 3).
Conclusion(s): This study outlines that RSS during the first two hours can be used as a predictor for need for surfactant administration. Optimal RSS cutoffs for early rescue surfactant administration need to be determined in large cohort studies.