Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 2: Physiology 1
338 - Development And Testing Of A Multifunction Feeding Tube Capable Of Respiratory, Cardiac And Temperature Monitoring
Publication Number: 338.345

Alan Groves, MBChB, MD (he/him/his)
Associate Professor
University of Texas at Austin Dell Medical School
Austin, Texas, United States
Presenting Author(s)
Background:
Respiratory support in preterm infants is increasingly provided by non-invasive methods. Continuous positive airway pressure (CPAP) provides a positive end expiratory pressure (PEEP) to the lungs but requires careful positioning and intensive nursing input. High flow nasal cannula (HFNC) is simpler to position but provides variable PEEP. All newborns requiring CPAP/HFNC have a gavage tube in place for routine clinical care. A pressure sensor placed within a gavage tube could provide continuous PEEP monitoring, potentially allowing titrated PEEP while receiving HFNC support. Additional sensors could allow quantification of work of breathing (transdiaphragmatic pressure gradient) and monitoring of heart rate and temperature.
Objective:
To develop a multifunction gavage tube capable of simultaneous pressure, temperature and ECG monitoring and to demonstrate feasibility of monitoring in an animal model equivalent in size to the preterm newborn.
Design/Methods:
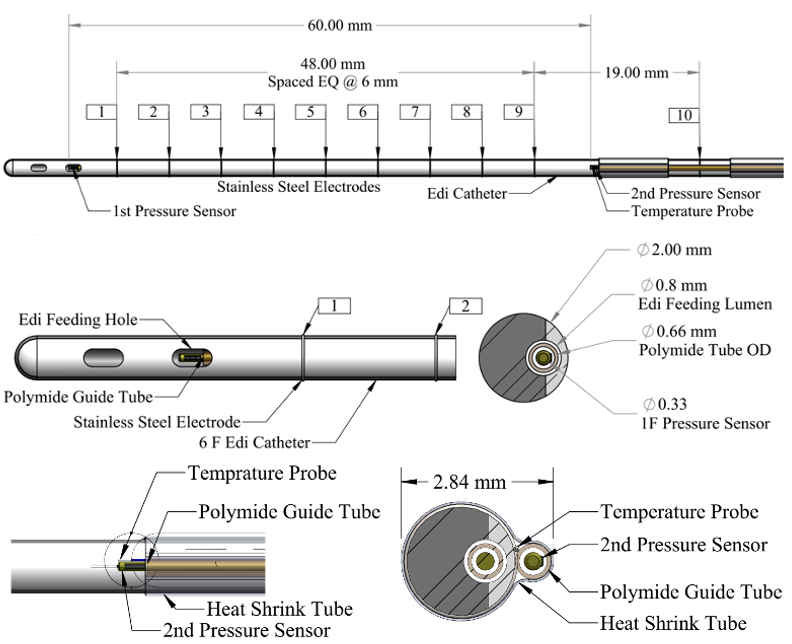
We inserted a 1Fr (0.33mm) pressure sensor (Millar, TX) within the lumen of a 6Fr (2mm) Neurally-adjusted ventilatory assist (NAVA) catheter (Getinge, Sweden) using a polyamide guide tube. A 2nd 0.33mm pressure sensor and a 0.13mm thermocouple (Omega Engineering, CT). were attached to the external surface 6cm from the catheter tip using heat shrink tubing (Fig 1). The total diameter of the device was 2.84mm. ECG signals were obtained from indwelling sensors at 2-7cm from the tip (Fig 1). The device was placed in an adult (722g) Sprague-Dawley rat (Charles River Laboratories, PA) under isoflurane anesthesia with IACUC approval. The tip of the tube was confirmed to be 2cm below the diaphragm by ultrasound. Pressure and temperature were recorded at frequency 10Hz, ECG at 250Hz. At the end of the experiment, the rat was euthanized by injection of potassium chloride.
Results:
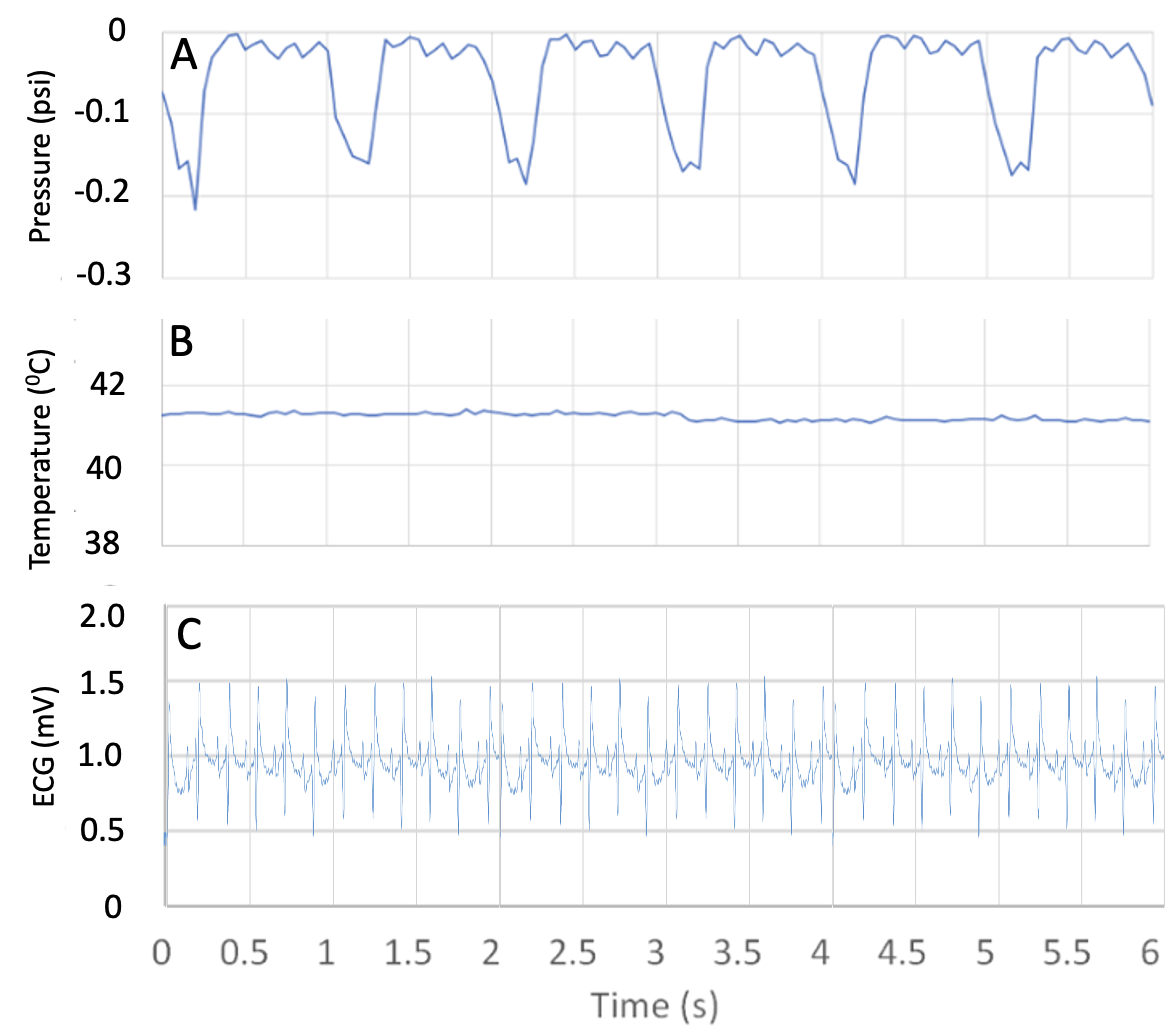
Reliable pressure signals at a range of 0-14 cm H2O (0-0.2psi) were obtained from pressure sensors placed both above and below the diaphragm (Fig 2A). A core temperature of ~410C was recorded (Fig 2B). Optimal ECG signals at a voltage range of 0-2mV were obtained from esophageal electrodes placed at 4 and 6cm from the tube tip, with ground placed at 9cm (Fig 2C).
Conclusion(s):
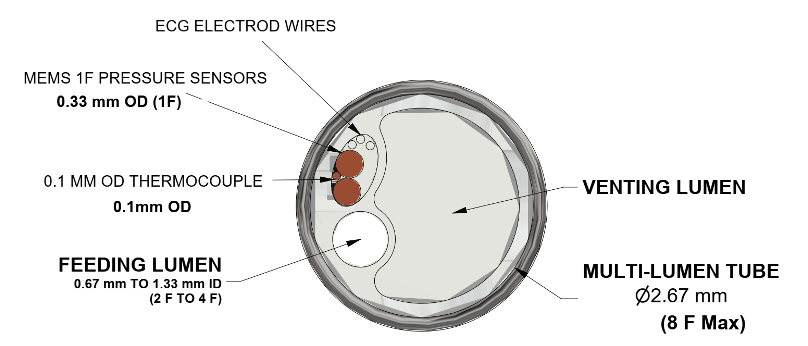
Our multifaction catheter provided continuous, reliable, high resolution esophageal pressure, temperature and ECG monitoring in an animal model equivalent in size to the preterm infant, with all sensors contained within a < 3 mm diameter tube as is routinely used in the preterm infant. A final version could contain these elements plus feeding and venting lumens in a device < 3mm in diameter (Fig 3).