Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 2
324 - Tidal volume levels after preterm birth: Gently does it
Publication Number: 324.348
- PP
Prue Pereira-Fantini, B. Sci (Hons), PhD (she/her/hers)
Senior Research Officer
Murdoch Children's Research Institute
Parkville, Victoria, Australia
Presenting Author(s)
Background: Tidal ventilation is essential in supporting the transition to air-breathing at birth, but excessive tidal volume (VT) is an important factor in preterm lung injury. There is limited information regarding the most lung protective tidal volume (VT) strategy to apply at birth, Most preterm lamb studies have used VT at 7 ml/kg however we have previously identified that a dynamic positive end-expiratory pressure (PEEP) strategy at birth, in which lambs are transiently exposed to a reduced VT of 3-5 ml/kg at 60-120s post-birth, reduces lung injury in preterm lambs compared to a static PEEP strategy. This raises the question as to whether the injury benefits were related to lower VT exposure, after a brief period of higher VT to aid aeration, rather than the higher PEEP.
Objective:
The objective of this study was to determine the role of different levels of VT during positive pressure ventilation (PPV) on initiating early lung injury pathways in the preterm lung.
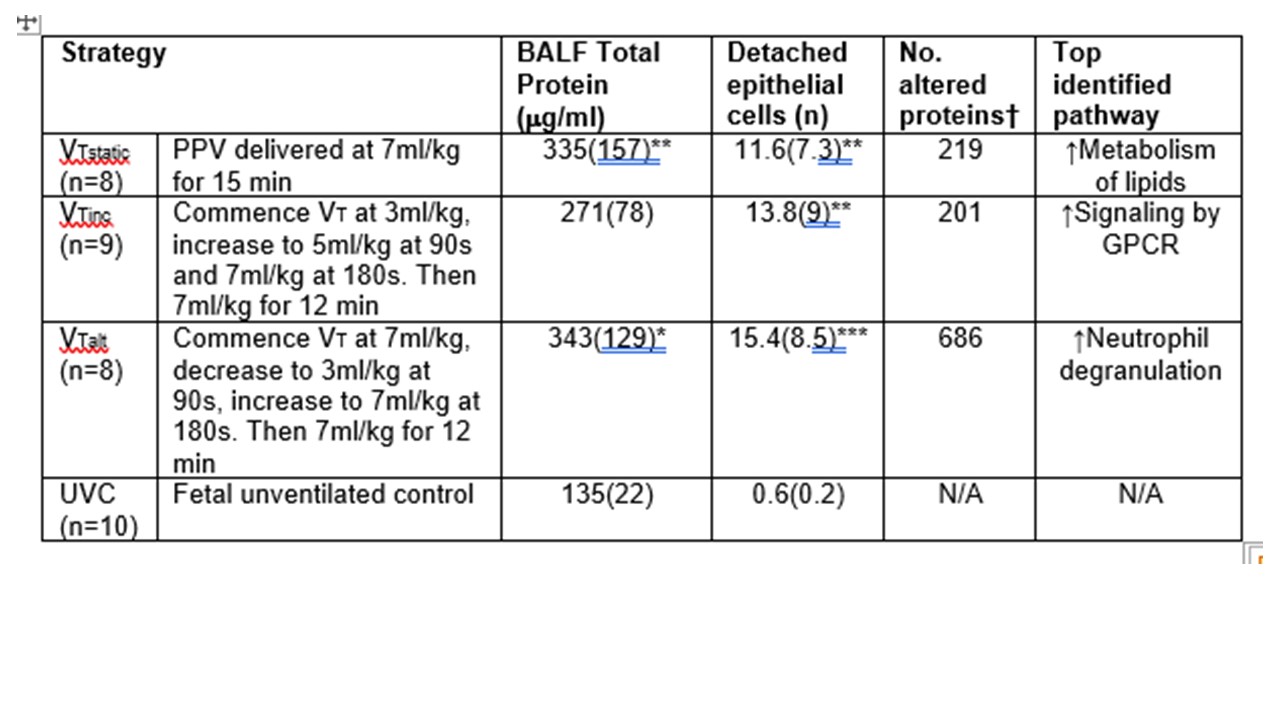
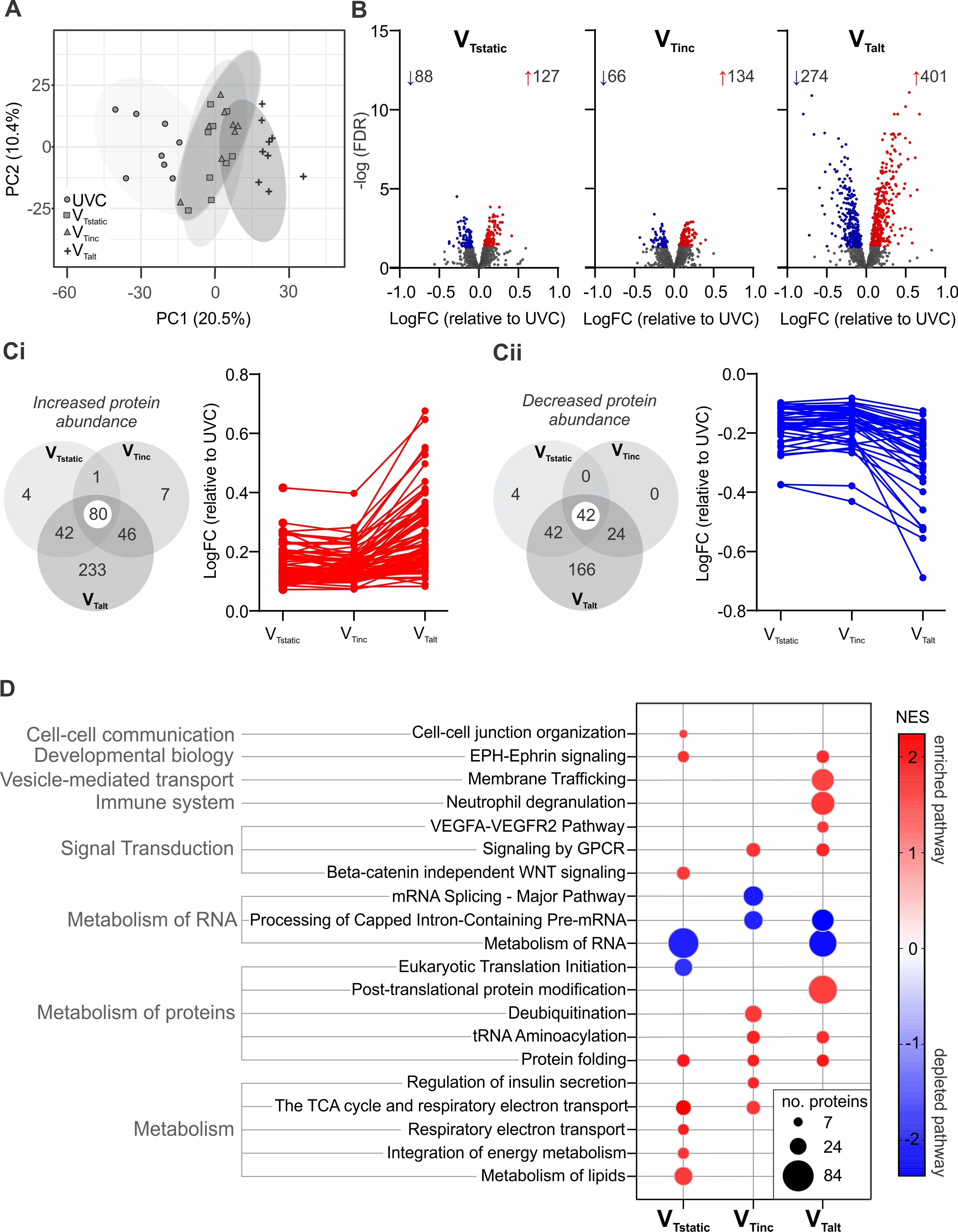
Design/Methods: 124-127d preterm lambs were randomly allocated to 15-min of volume-targeted PPV with different VT levels in the first 3 min after birth (Table 1). Lung mechanics and volumes (using electrical impedance tomography) were measured throughout, and lung injury assessment performed on post-mortem samples (using histology, BALF total protein concentration, and mass spectrometry-based proteomics).
Results: Lung injury and proteome results presented in Table 1. VT, inflating pressure, lung compliance and end-expiratory volume (aeration) were similar in all groups from 4 min, as was histology and BALF concentration. The transient decrease in VT in the VTalt group caused increased ventilation heterogeneity. From the 1610 proteins identified in the lung, 3-fold more proteins were altered with VTalt compared with VTstatic or VTinc strategies (Figure 1). Gene set enrichment analysis identified different biological processes, cellular components and pathways enriched in each strategy including increased immune activation associated with VTalt.
Conclusion(s): Our finding of comparable lung physiology and volutrauma across VT groups challenges the paradigm that there is a need to rapidly aerate the preterm lung at birth. Increased lung injury and ventilation heterogeneity was identified when initial high VT was suddenly decreased during respiratory support at birth, further supporting the benefit of a gentle VT approach.