Neonatal General
Neonatal General 7: NICU Practices 1
177 - Impact of NICU Provider Type on In-hospital Respiratory Outcomes of VLBW Infants
Publication Number: 177.331

Andrew Berenz, MD (he/him/his)
Assistant Professor
Rush University Medical Center
Chicago, Illinois, United States
Presenting Author(s)
Background:
Practice variation exists in the early postnatal management of very low birth weight (VLBW) infants and has been shown to result in adverse outcomes. This has led to the development of “small baby” units with focus on quality improvement initiatives to enhance the outcome of these infants. These practices include the assignment of the smallest VLBW patients to advanced practice providers (APPs) specialized in the care of preterm infants as opposed to pediatric residents who rotate once a year through the NICU. Currently, there is a paucity of data comparing outcomes of VLBW infants cared for by APPs as compared to residents.
Objective:
To examine the impact of provider types in the first 14 days of life on in-hospital respiratory outcomes in VLBW infants.
Design/Methods:
This is a single-center review of all VLBW (< 1500 g) infants born from Jan 2016 through Dec 2020, admitted to an academic tertiary NICU. Exclusion criteria; admission after 48 hours of life, early neonatal death (< 14 days). Infant-level perinatal characteristics and in hospital morbidities were collected as were details of provider-level care oversight. Respiratory outcomes including the level of support at 14, 28 days and at 36 weeks postmenstrual age were collected. To evaluate the impact of provider level care on respiratory outcomes, logistic regression models were created to control for confounding variables at the predefined time points.
Results:
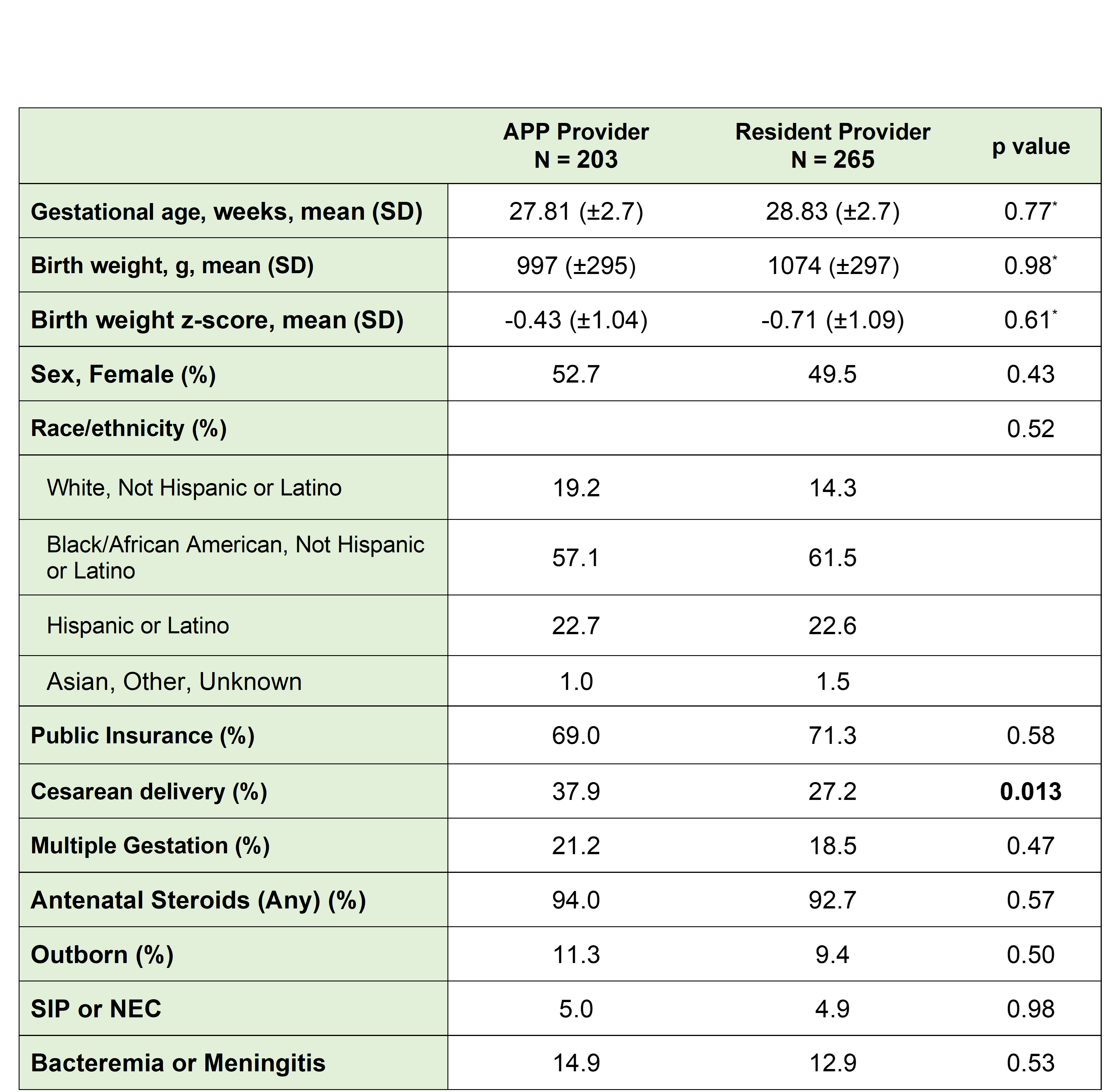
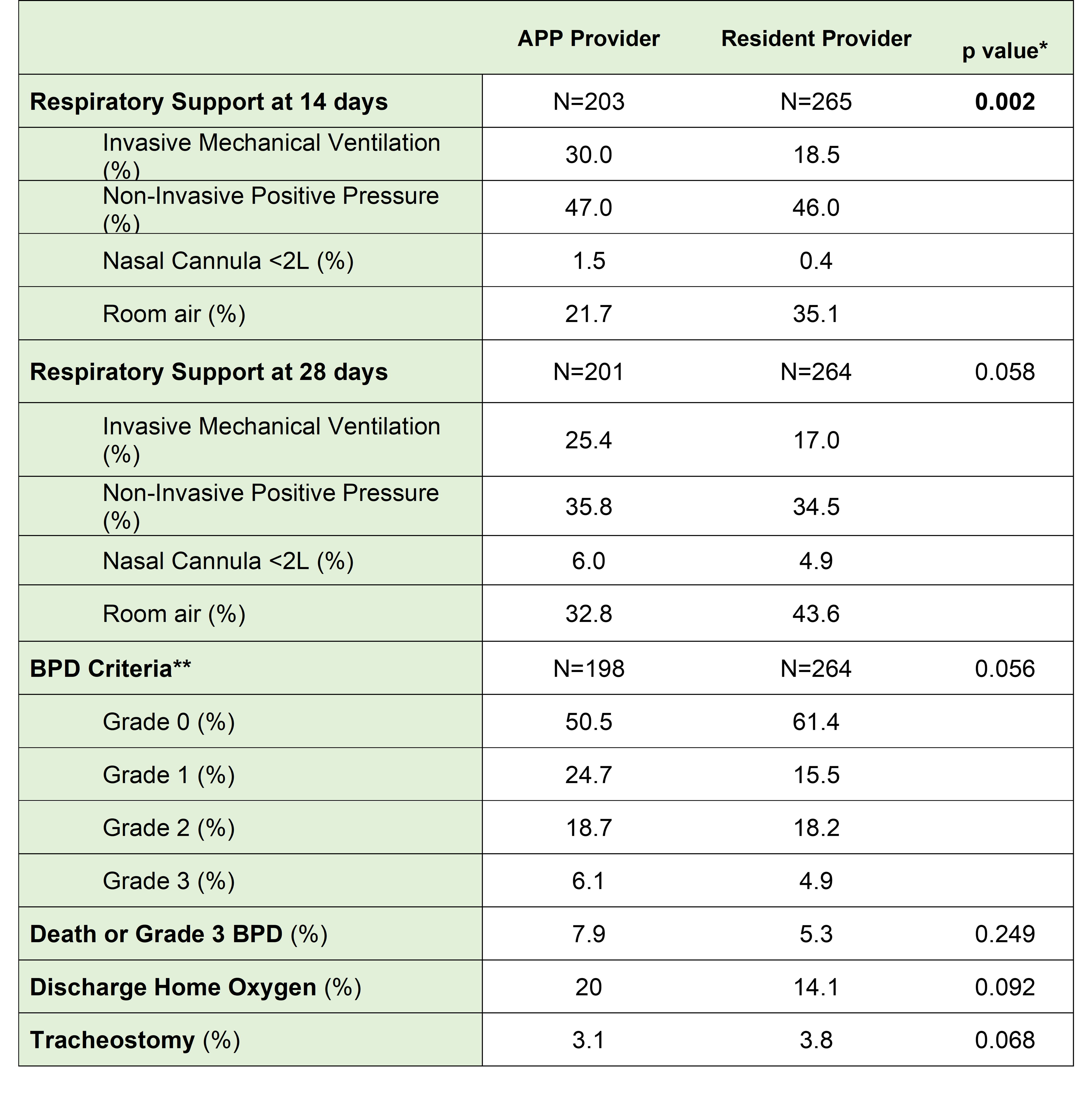
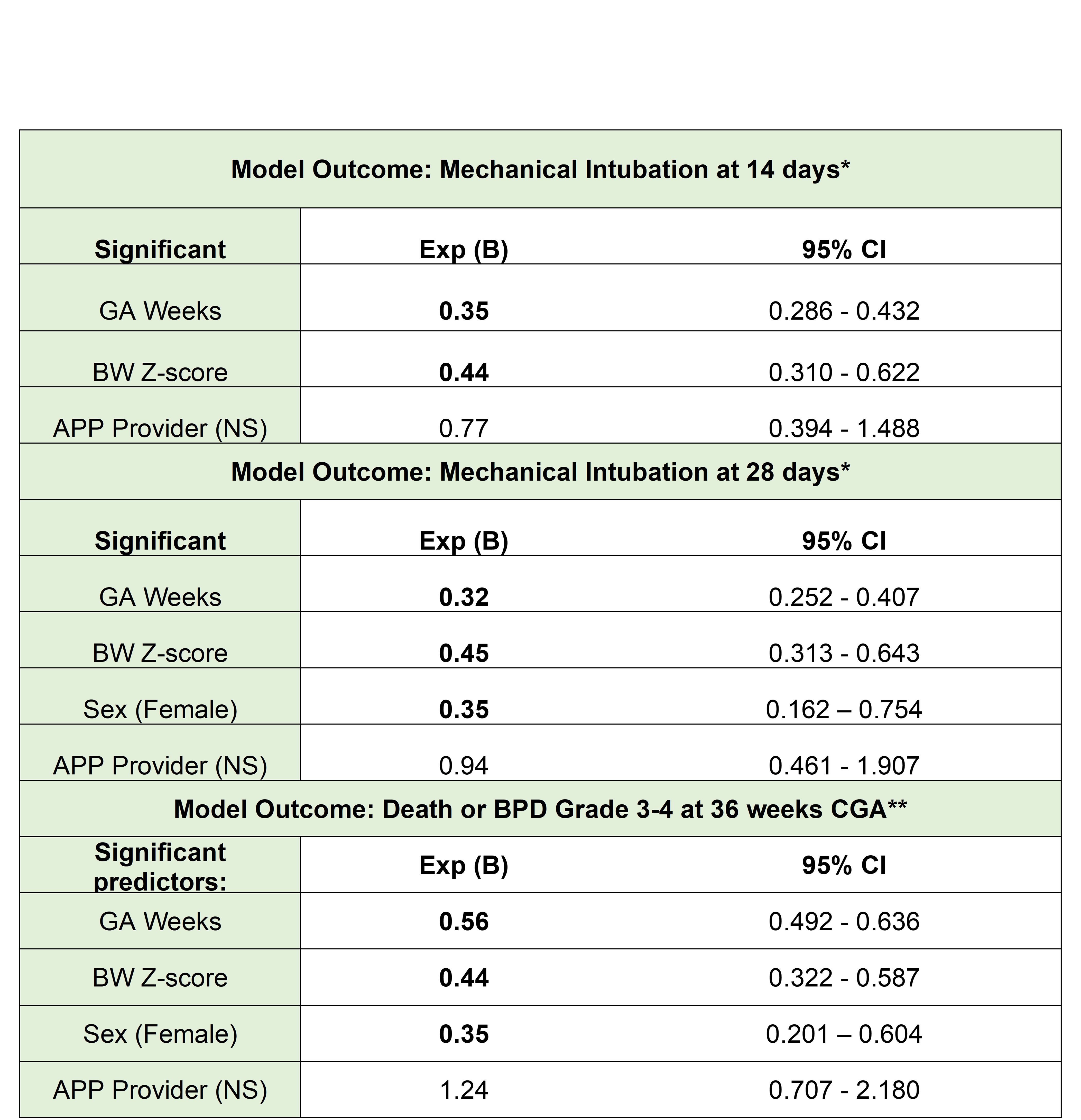
468 VLBW infants met inclusion criteria. infants cared for by APPs were more likely to be delivered by c-section (38 vs 27%, p = 0.013). All other characteristics were similar (Table 1). There were significant differences in respiratory support at 14 days with APP patients more likely to receive mechanical ventilation (25% vs 17%)(Table 2). Regression models accounting for known and identified risk factors for respiratory morbidity demonstrated no interaction of provider type (APP vs resident) on the respiratory outcomes (Table 3).
Conclusion(s):
VLBW patients cared for by APPs in our center had higher likelihood of remaining intubated at 14 days of life. However, when accounting for other risk factors of respiratory morbidity in this population, no association was observed between provider type and need for mechanical ventilation at 14 or 28 days, or death or severe BPD at 36 weeks.
Ideal staffing models for the optimal care of VLBW infants remain unclear. The impact of mid-level provider type and attending-level characteristics will be analyzed for in-hospital outcomes in addition to neurodevelopment and healthcare utilization for VLBW infants.