Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 1: Lung US - BPD
294 - Volume-guarantee versus pressure-limited ventilation in the first two weeks of life and development of bronchopulmonary dysplasia in extremely premature infants
Publication Number: 294.344
- MC
Milenka Cuevas Guaman, MD (she/her/hers)
Assistant professor
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background:
Extremely premature infants (EPI) are at high risk for developing bronchopulmonary dysplasia (BPD). Although volume-targeted ventilation (VTV) has been shown to be beneficial in preventing BPD, scarce data exists to guide ventilator management of infants with evolving BPD. Some include time-cycled pressure-limited ventilation (PLV) and more recently volume-guarantee ventilation (VGV) (a form of VTV). In our first study, we found that use of PLV as opposed to VGV in EPIs with evolving BPD (DOL 21, 28) was associated with higher rates of BPD at 36 weeks PMA. This observation prompts the question of whether the use of PLV as opposed to VGV in the first week of life of EPIs is associated with higher rates of BPD at 36 weeks PMA.
Objective:
To determine the association between type of ventilation (VGV vs. PLV) of EPIs on DOL 7 and DOL 14 with death and/or BPD at PMA 36 weeks as defined by the Vermont Oxford Network.
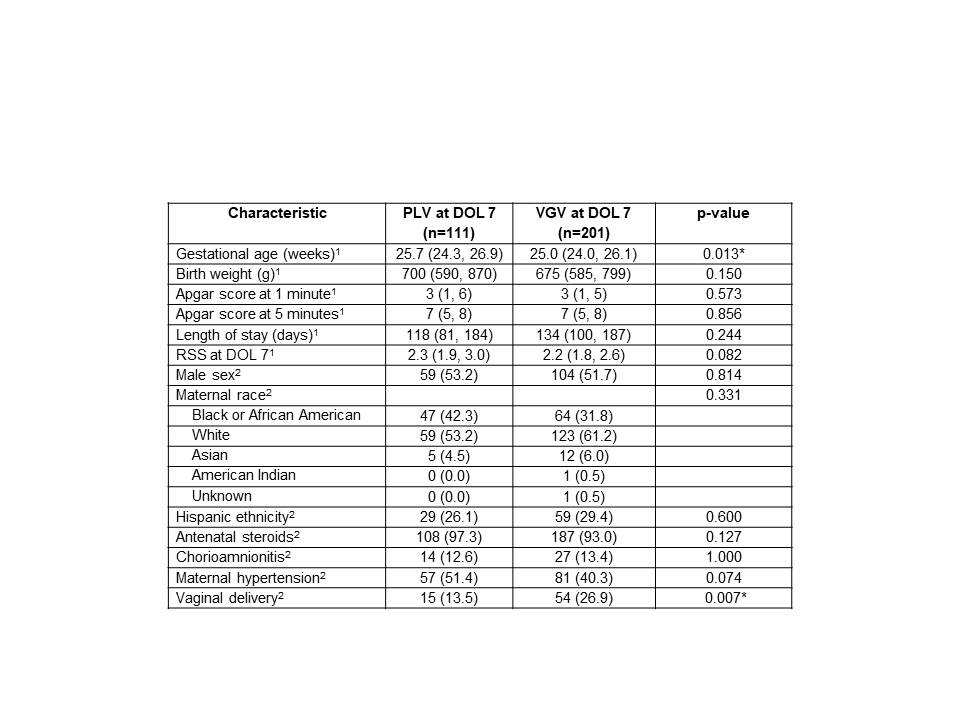
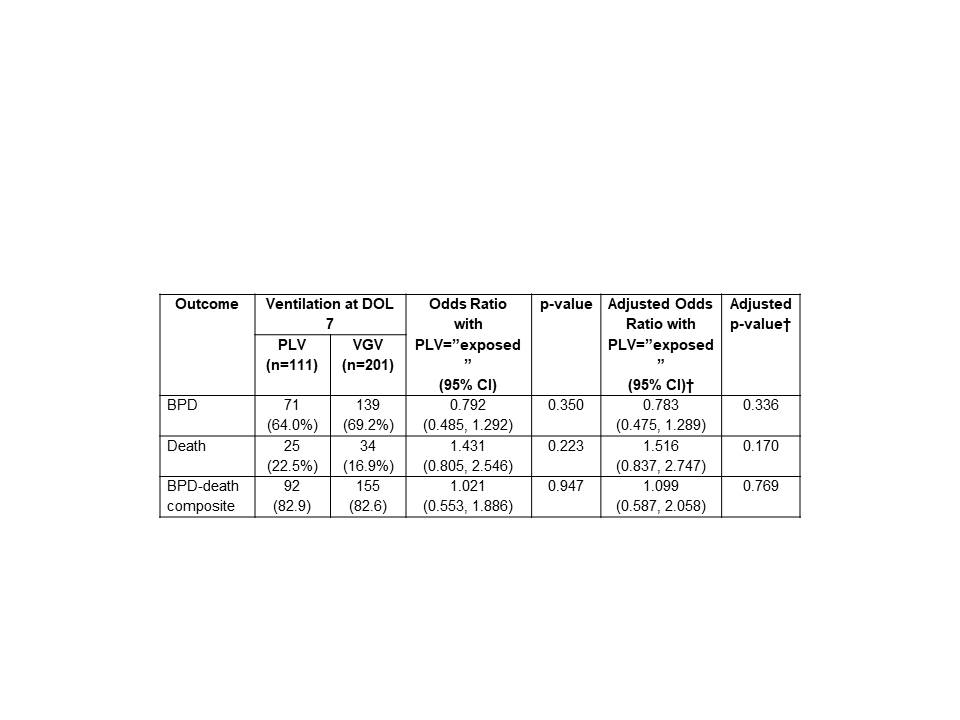
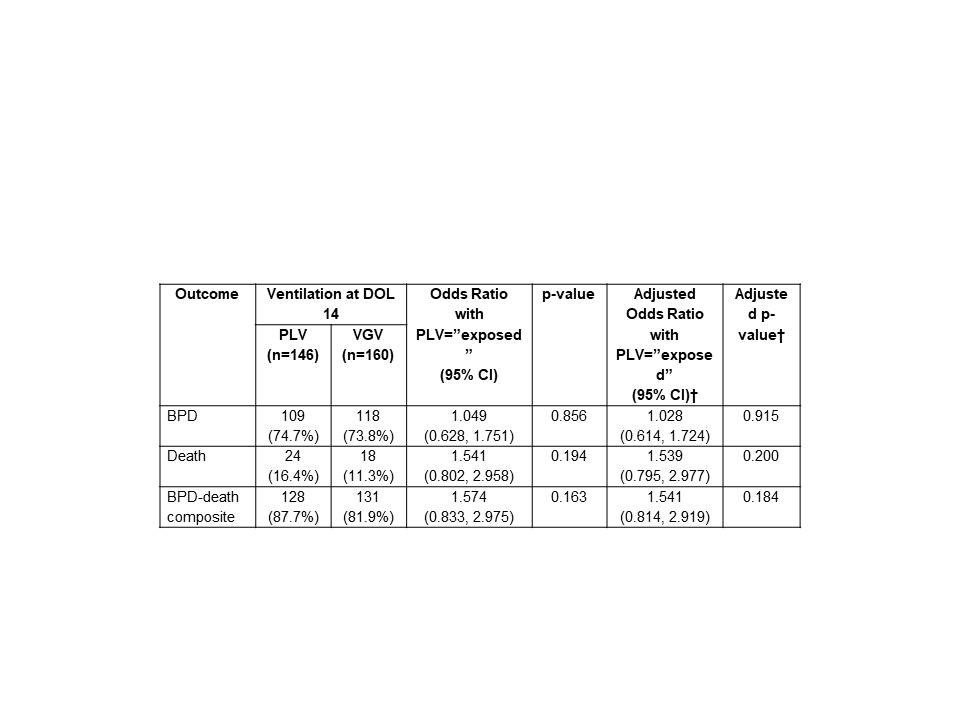
Design/Methods: Single-centered, retrospective cohort review of medical records of premature infants less than 28 weeks admitted to a Level 4 NICU from January 2012 to December 2021. Data abstracted included: demographics, maternal and birth data, and ventilator data and respiratory severity score (RSS) at DOL 7, DOL 14 until death or discharge. Logistic regression was used to compare odds of BPD, death and a BPD-death composite for patients exposed to PLV versus VGV at DOL 7 and 14. Unadjusted comparisons were made in addition to comparisons after controlling for characteristics that differed significantly for patients exposed to PLV versus VGV at DOL 7.
Results:
At DOL 7 there were 111 patients exposed to PLV and 201 patients exposed to VGV. At DOL 14 there were 146 patients exposed to PLV and 160 patients exposed to VGV. Patient characteristics for those exposed to PLV vs VGV are compared in Table 1. There were no significant differences in outcomes for patients on PLV vs VGV at DOL 7 (Table 2) or DOL 14 (Table 3).
Conclusion(s):
Our study demonstrates no association of use of VGV vs PLV at DOL 7 or 14, in contrast with our prior study results at DOL 21 and 28 with decreased risk of BPD with the use of VGV compared to use of PLV. This points to a critical window between DOL 14 and 21. Prospective trials are needed to further delineate the most effective ventilatory modality for this population with ‘evolving’ BPD.