Neurology: Neurodevelopment
Neonatal Neurology 5: Clinical
117 - Serial Neuroimaging and Term-equivalent Age Neurodevelopmental Outcomes of Very Preterm Infants Receiving Tailored Neuropromotive Support in the NICU
Publication Number: 117.337

Danielle Sharon, BS (she/her/hers)
Clinical Research Assistant
Brigham and Women's Hospital, United States
Gabriel Cote Corriveau, MD
Research Fellow
Department of Pediatric Newborn Medicine, Brigham and Women’s Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Co-Author(s)
Background: Infants born very preterm (VP) undergo rapid brain growth and development prior to term-equivalent age (TEA) while in the neonatal intensive care unit (NICU), a critical window for intervention. Early MRI imaging has the potential to identify infants with neurological injury and may help tailor early neuropromotive interventions to optimize neurodevelopmental outcomes while in the NICU prior to TEA.
Objective:
Use early MRI to stratify VP infants into low-risk or high-risk groups based on degree of brain injury and tailor rehabilitative intervention according to risk category.
Explore associations between rehabilitative intervention, total and regional brain growth and short- and long-term outcomes of preterm infants.
Design/Methods:
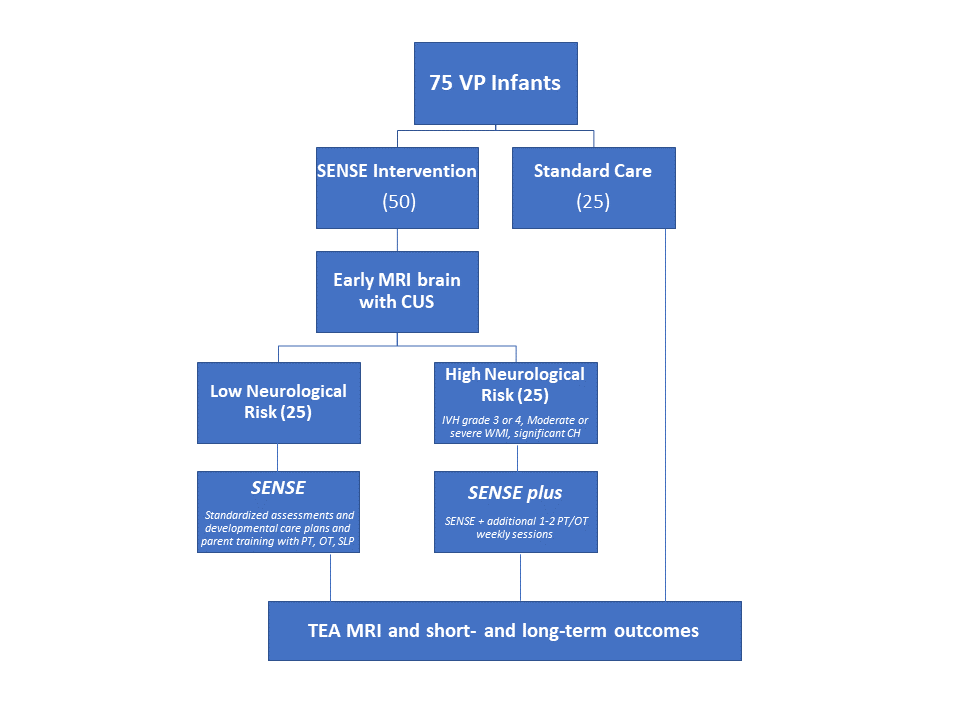
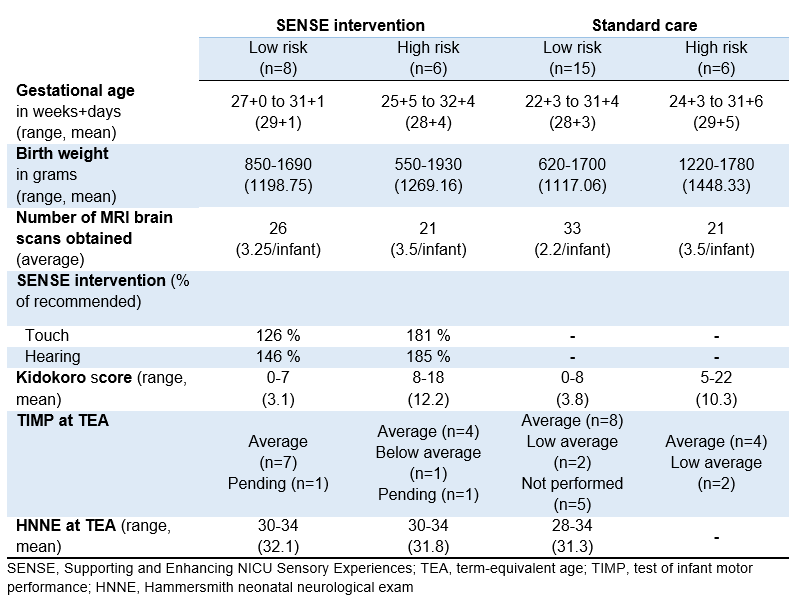
This is a prospective study of 75 infants born < 33 weeks gestation age (GA), weighing between 0.5-4.5 kg and without any congenital infections or anomalies, in a level-III NICU. Infants assigned to the intervention group are stratified into low- and high-risk groups based on early MRI and compared with a standard of care group (Figure 1). The intervention is based on the Supporting and Enhancing NICU Sensory Experiences (SENSE) program, with tailored weekly multisensory plans intended to be implemented preferentially by parents with staff and developmental therapists’ support. For infants in the high-risk group, the SENSE program is enhanced with additional motor and other developmental therapy (SENSE-plus). Serial MRIs are obtained at least three times until TEA, along with routine cranial ultrasound (CUS) per unit guidelines. At TEA, MRI scans are scored using the Kidokoro system and neurodevelopmental status is assessed by test of infant motor performance (TIMP) and Hammersmith neonatal neurological exam (HNNE) score.
Results:
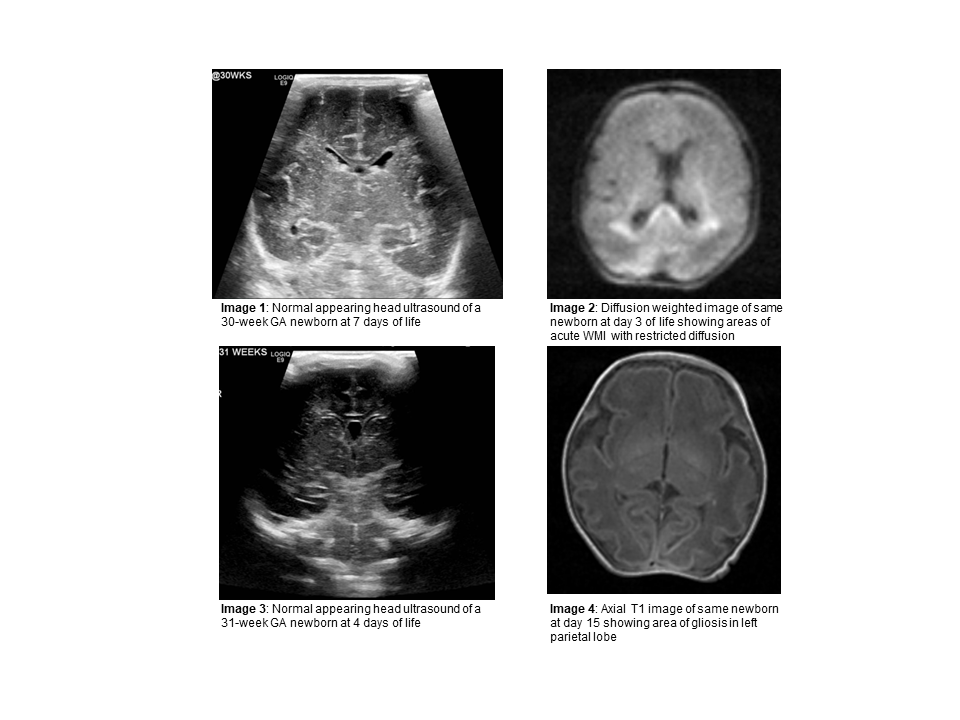
To date, 35 infants (of projected 75) have been enrolled, including 14 intervention (8 low-risk and 6 high-risk) and 21 standard care participants. Of the 101 MRIs performed, 39 were early (30-34 weeks GA) scans. Early MRI identified 11 high-risk infants, as opposed to 7 based on CUS only (Figure 2). MRI detected more white matter injuries (WMI) (6 vs 3 moderate-severe WMI; 12 vs 4 for any WMI) and cerebellar hemorrhages (3 vs 2) than CUS. Participants assigned to the intervention groups received 75% or more of the intended multisensory experiences (Table 1). Long term outcome analysis is underway.
Conclusion(s):
A targeted neuropromotive intervention informed by early brain MRI is feasible and has the potential to improve outcomes of infants born very preterm.