Neonatal Neurology: Clinical Research
Neonatal Neurology 6: Clinical 6
131 - No Difference in Shunt Complications and Outcomes in Posthemorrhagic Hydrocephalus Infants With or Without Temporizing Procedures: Analysis of National Surgical Quality Improvement Program (NSQIP)
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 131
Publication Number: 131.338
Publication Number: 131.338
Erwin T. Cabacungan, Medical College of Wisconsin, Wauwatosa, WI, United States; Samuel J. Adams, Children's Hospital of Wisconsin, Milwaukee, WI, United States; Katherine A. Carlton, Medical College of Wisconsin, Mequon, WI, United States; Andrew B. Foy, Medical College of Wisconsin, Milwaukee, WI, United States; Avantika Singh, Medical College of Wisconsin, Milwaukee, WI, United States; Susan S. Cohen, Medical College of Wisconsin, Milwaukee, WI, United States

Erwin T. Cabacungan, MD, MPH
Associate Professor
Medical College of Wisconsin
Wauwatosa, Wisconsin, United States
Presenting Author(s)
Background: Permanent cerebrospinal fluid (CSF) shunt placement in premature infants with posthemorrhagic hydrocephalus (PHH) is associated with severe complications and poor outcomes. Temporizing procedures (TP) are increasingly used for the goal of shunt prevention. Nonetheless, many infants with TP still require CSF shunts. Practice variation exists, and it is unknown if these TP reduce complications and improve outcomes. Collaborative quality improvement databases offer the ability to examine practices and compare outcomes.
Objective: To compare complications and outcomes of PHH infants receiving their first CSF shunt.
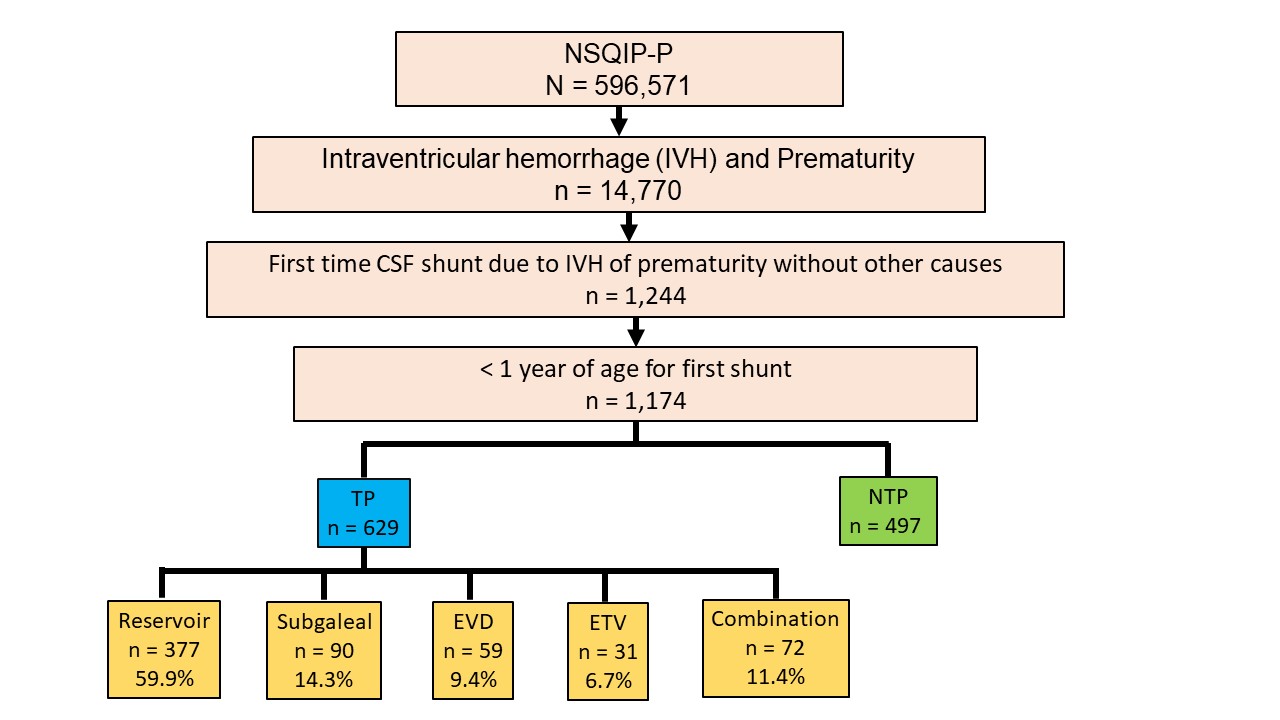
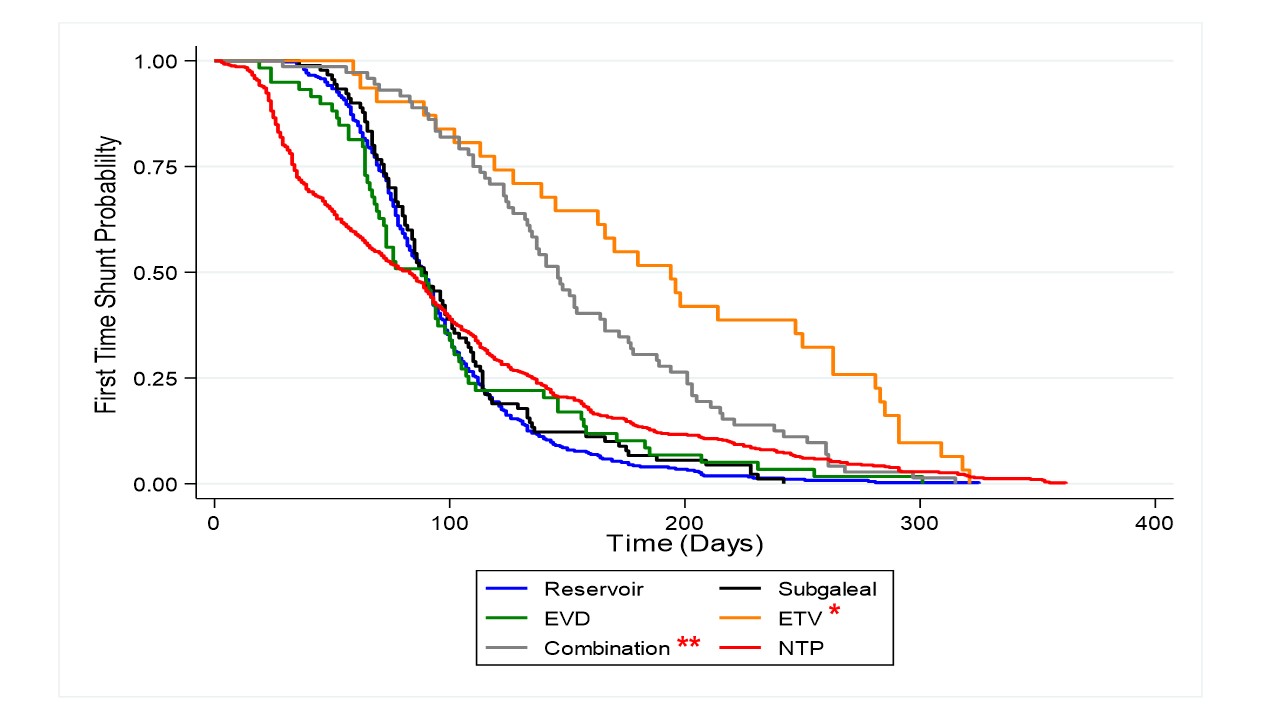
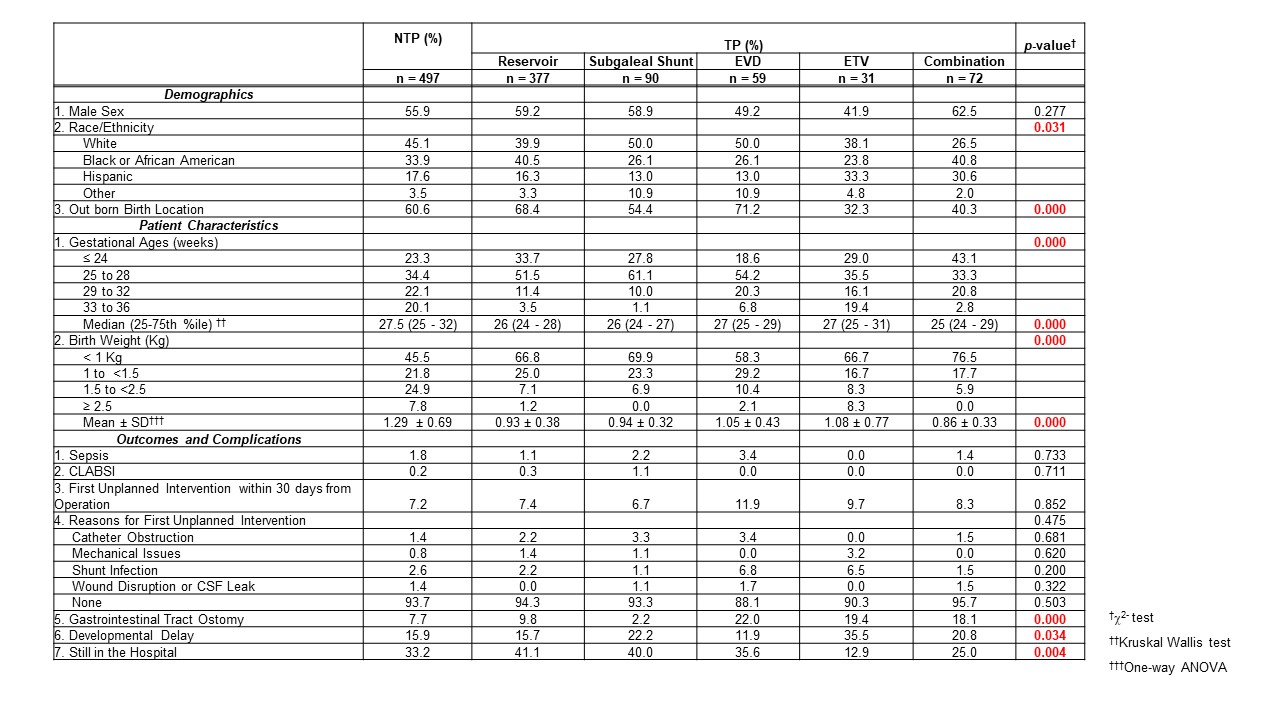
Design/Methods: This is a retrospective cohort study of PHH infants who underwent their first CSF shunt using the 2016 -2020 NSQIP Pediatric CSF procedure-targeted dataset. The predictor variable was primary neurosurgical intervention types: no prior temporizing procedures (NTP) vs. prior TP (reservoir, subgaleal, external ventricular drainage (EVD), endoscopic third ventriculostomy w/ or w/o choroid plexus coagulation (ETV) and combination). Patient characteristics, complications, and outcomes were collected. Kaplan-Meier survival curves showed differences in the timing of shunt placement between the groups. Statistical analysis included Chi-square, Kruskal Wallis, One-Way ANOVA, and Cox proportional hazard regression.
Results: NSQIP dataset included 596,571 infants, and 2.5% of infants were premature and had PHH (Figure 1). Majority of infants received TP (54%; Figure 1), with ventricular reservoir being the most common procedure performed (60%). The median gestational age at birth for this cohort was 25-27.5 weeks (Table 1). Compared to NTP infants, infants receiving a combination of TP prior to shunt were younger and smaller at birth. Infants with ETV procedures were twice as old at time of shunt procedure compared to NTP infants (83 days vs. 194 days, Figure 2). The Hazard ratio for ETV was 0.51 compared to NTP (p< 0.05). No differences were seen in rates of sepsis, central line infections, shunt infections, or shunt mechanical issues. Infants with EVD, ETV, and combination procedures required gastrostomy tubes more frequently. More developmental delays were seen in infants with ETV (p< 0.05).
Conclusion(s): The only procedure associated with delayed CSF shunt procedure was ETV, but ETV was associated with more feeding issues and developmental delays. Our results suggest that shunt placement, with or without TP, had similar complications and outcomes in this large national dataset.