Neonatal Follow-up
NICU Follow Up and Neurodevelopment 5: Impact of Parents and Social Determinants of Health
161 - Early Neurobehavioral and Medical Risks associated with 3 year Developmental Outcomes among Preterm Born Infants
Publication Number: 161.363

Elisabeth McGowan, MD (she/her/hers)
Women & Infants Hospital of Rhode Island
Providence, Rhode Island, United States
Presenting Author(s)
Background:
Recent data suggest that atypical neonatal neurobehavioral patterns predict both adverse developmental outcomes as well as significant behavioral problems at 2 years. The combined contribution of neurobehavioral and medical risk on 3-year outcomes has yet to be studied.
Objective:
Determine associations between neonatal neurobehavior utilizing NICU Network Neurobehavioral Scale (NNNS), neonatal medical risk, and 3-year outcomes.
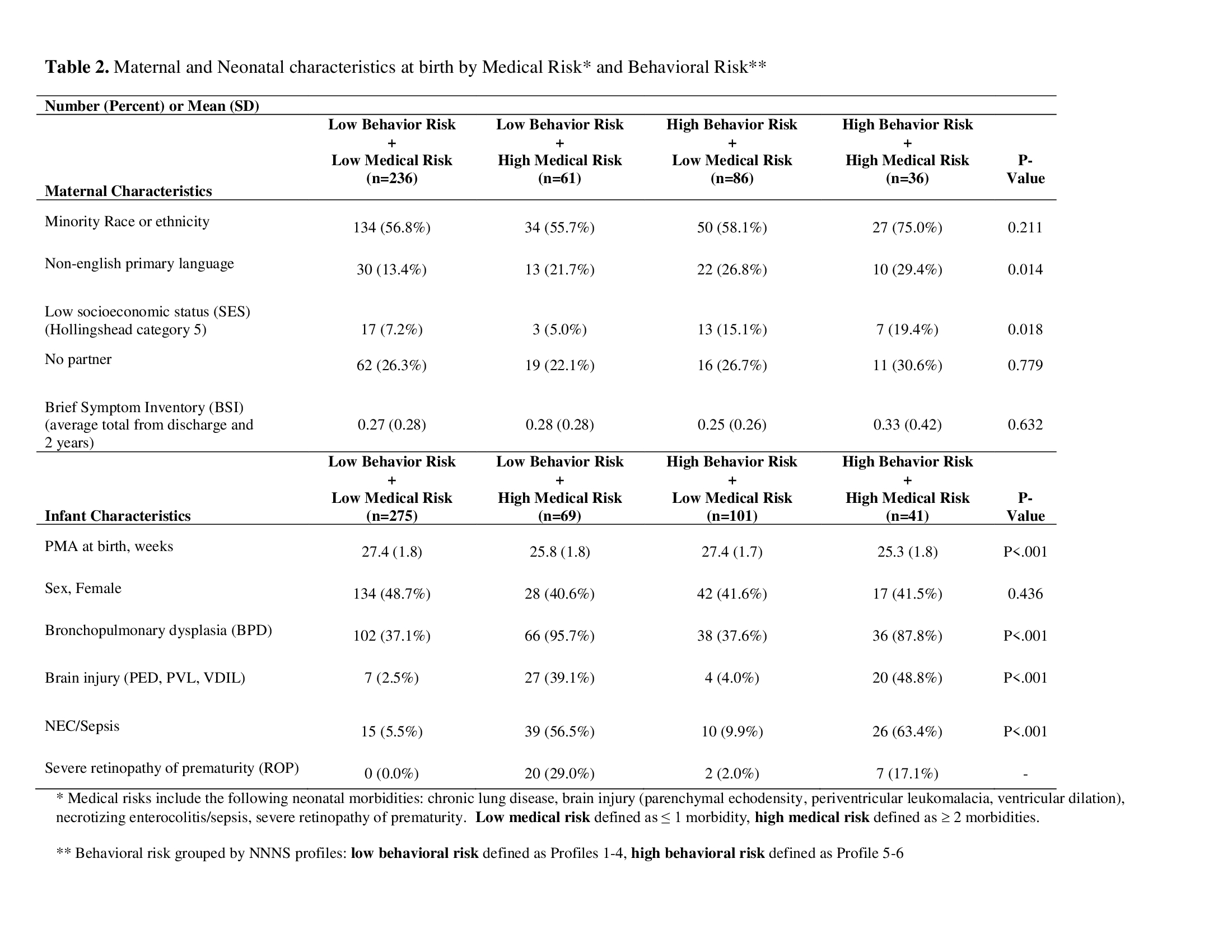
Design/Methods: Multi-center study of 704 infants born < 30 weeks gestation enrolled in the Neonatal Neurobehavior and Outcomes in Very Preterm Infants (NOVI) Study. NNNS were completed prior to NICU discharge and six profiles of neonatal neurobehavior were calculated by latent profile analysis. Medical morbidities included brain injury, chronic lung disease, retinopathy of prematurity, and necrotizing enterocolitis/sepsis. Outcomes at 3 years were Bayley Scales of Infant and Toddler Development-III (Bayley-III) composite scores and Child Behavior Checklist (CBCL) T-scores. Generalized estimating equation models were used to test the associations among NNNS profiles, neonatal medical risk, and 3-year developmental outcomes, while accounting for multiple births. Covariates were site, maternal socioeconomic status, race or ethnicity, maternal primary language, partner status, maternal psychopathology, and infant sex.
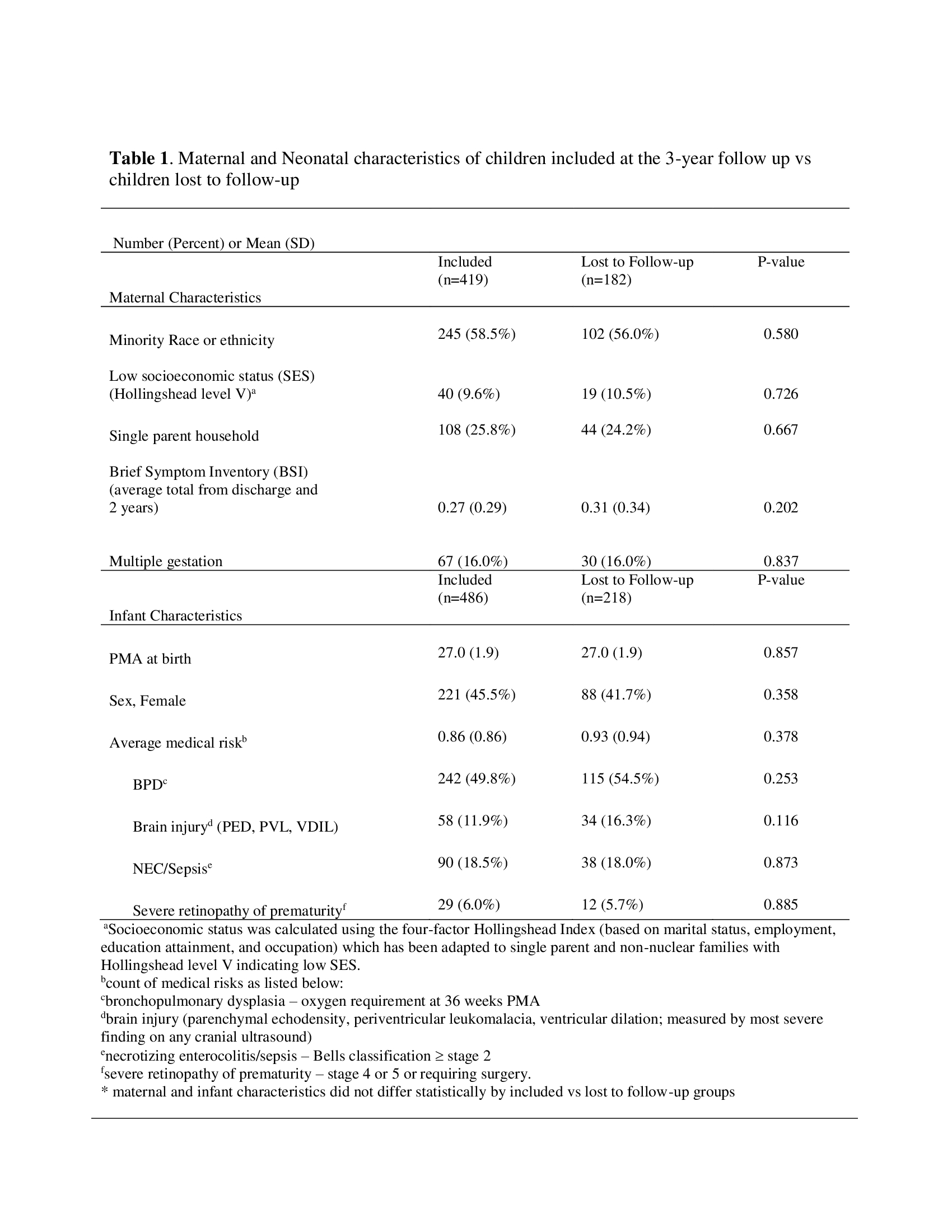
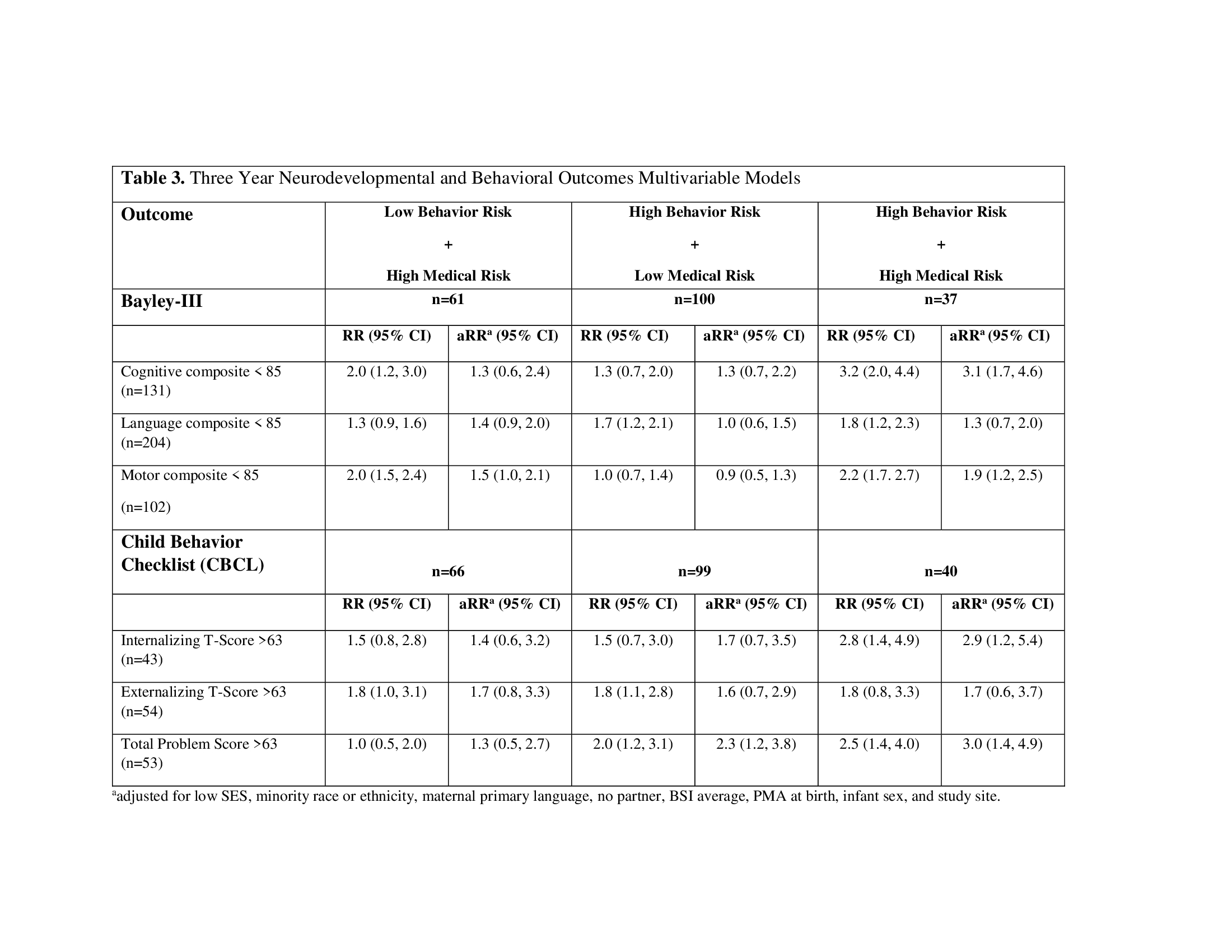
Results: 3-year follow-up data were available for 419 mothers and 486 infants (Table 1). Two NNNS behavior profiles were considered high behavioral risk (n=142). Infants with ³ 2 medical morbidities were considered high medical risk (n=110); 275 infants were both low behavioral and low medical risk (Table 2). High behavioral/low medical risk (n=99) infants were more likely to have clinical range for CBCL Total Problem scores (aRR 2.3; 95% CI: 1.2, 3.8) compared to low behavioral/low medical risk infants. High behavioral/high medical risk infants (n=37) were more likely to have Bayley-III cognitive and motor scores < 85 (aRR 3.1; 95% CI: 1.7, 4.6 and aRR 1.9; 95% CI: 1.2, 2.5) as well as clinical range CBCL (n=40) Internalizing and Total Problem scores (aRR 2.9; 95% CI: 1.2, 5.4 and aRR 3.0; 95% CI: 1.4, 4.9) compared to low behavioral/low medical risk infants (Table 3).
Conclusion(s): High risk NNNS profiles at NICU discharge add significant diagnostic and prognostic information concerning adverse outcomes through 3 years of age. In conjunction with medical risk, neurobehavioral assessments enhance identification of cognitive, motor and behavioral risk for delay.