Neonatal Respiratory Assessment/Support/Ventilation
Neonatal Respiratory Assessment/Support/Ventilation 3: Physiology 2 and Clinical Outcomes
349 - Methods for monitoring and definitions of apneas in preterm infants: a scoping review
Publication Number: 349.346
.jpeg.jpg)
Emily M. Jeanne (she/her/hers)
M.Sc. Candidate
McGill University, Faculty of Medicine and Health Sciences Montreal, Quebec, Canada
Montreal, Quebec, Canada
Presenting Author(s)
Background: Apneas are ubiquitous in preterm infants and are associated with complications. Adequate detection and differentiation between central, obstructive, and mixed apneas requires simultaneous monitoring of respiratory efforts and airflow. However, apnea monitoring practices and definitions remain unstandardized.
Objective: To describe the clinical methods used to monitor apneas and definitions employed in preterm infants hospitalized or recently discharged from the NICU.
Design/Methods:
In this scoping review, MEDLINE, Embase, Web of Science, and Cochrane Library were systematically searched. Studies published between 01/2000 and 12/2021 involving continuous physiological monitoring of apneas during NICU hospitalization or within 4 weeks from NICU discharge amongst infants < 37 weeks’ gestation were included. Study characteristics, devices employed for apnea detection and their respective accuracies, and apnea definitions were described.
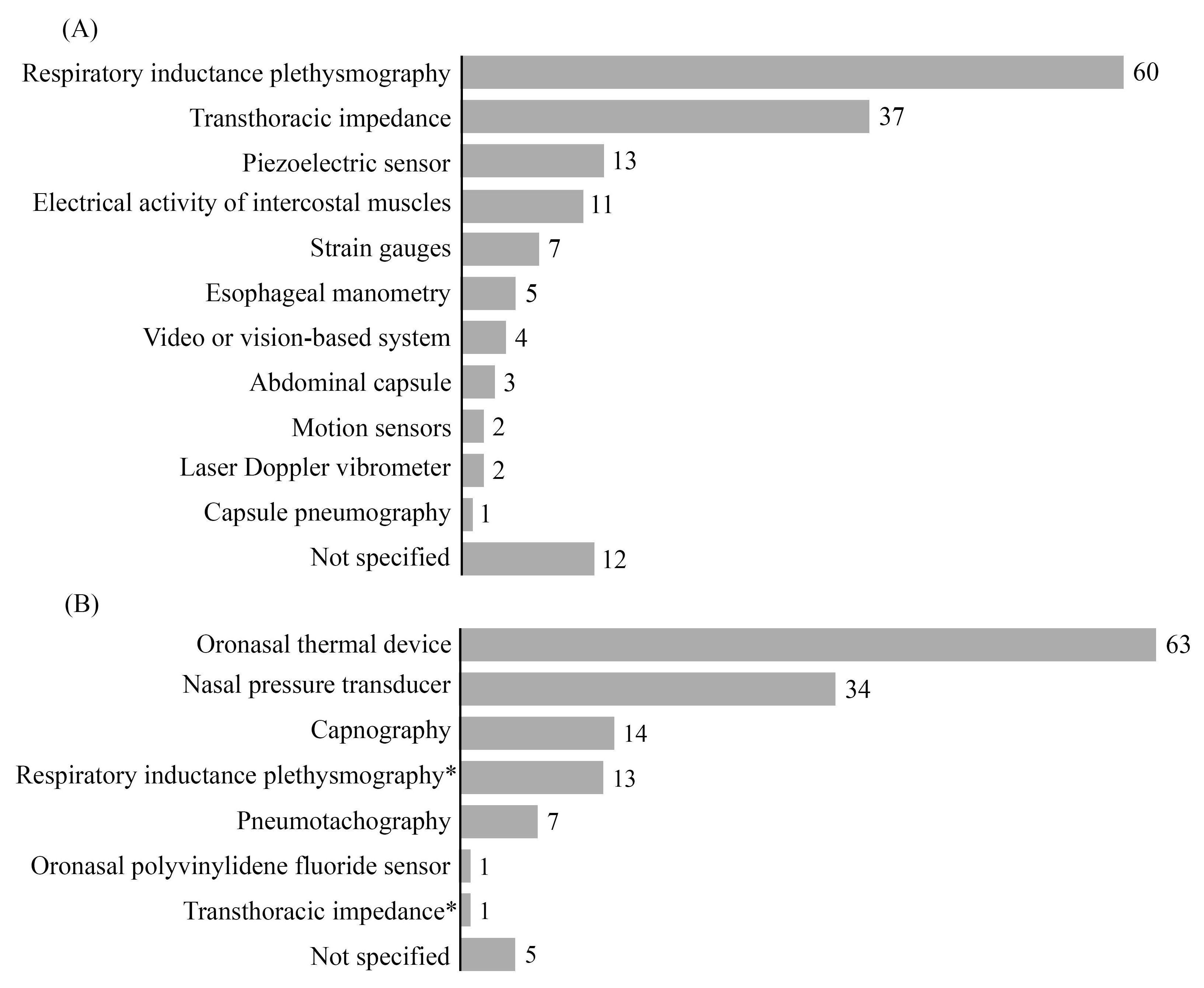
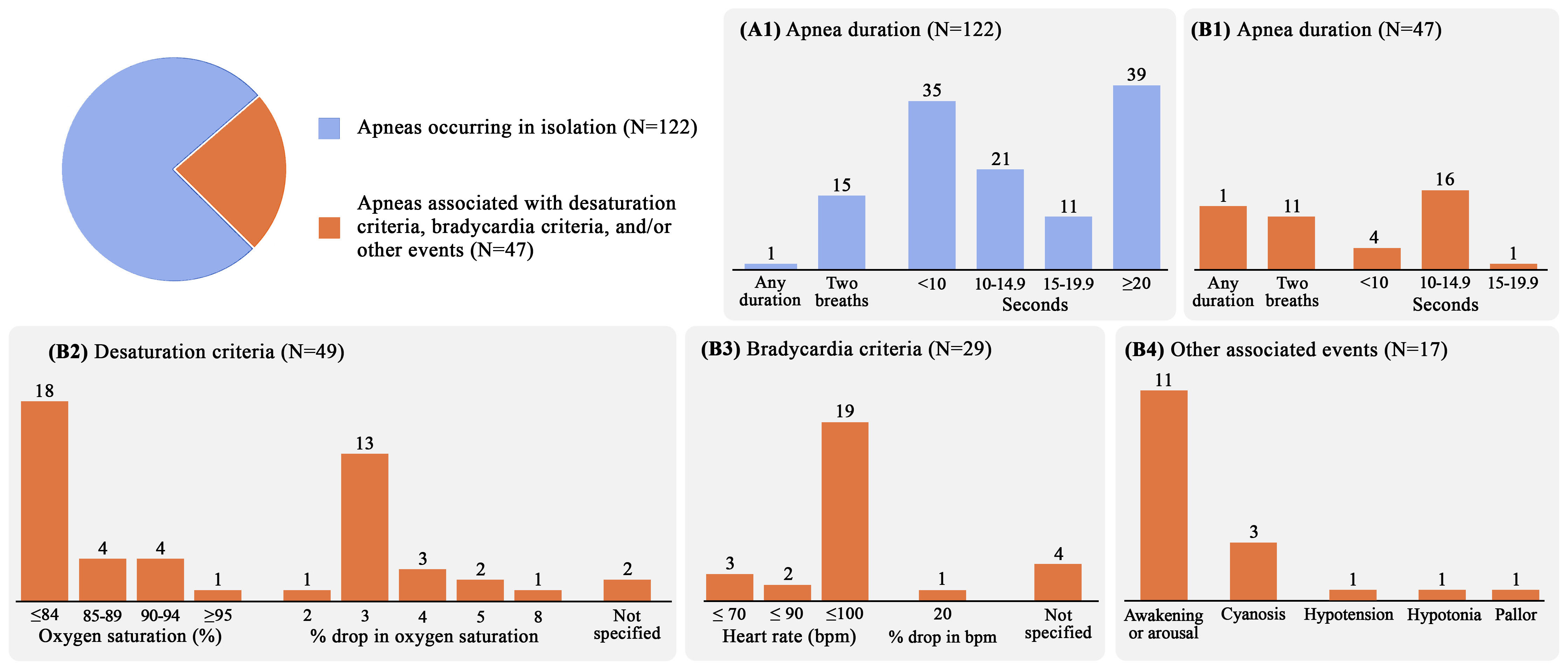
Results: 148 studies were included (Table 1). Monitoring was mostly done during hospitalization (n=117, 79%), for a median duration of 6h (IQR 3-11h). Eleven distinct devices were employed to monitor respiratory effort, with the most common being respiratory inductance plethysmography (n=60), transthoracic impedance (n=50), and piezoelectric sensors (n=13) (Fig 1). Conversely, 7 different devices were used to monitor airflow, with oronasal thermal devices (n=63), nasal pressure transducers (n=34), and capnography (n=16) the most common. Accuracy in detecting central apneas was mostly evaluated by transthoracic impedance (n=10), demonstrating sensitivities ranging from 9% (used alone) to 95% (used with an algorithm filtering the integrated bedside signals). Sensitivities in detecting obstructive apneas were reported as: nasal pressure transducers = 95%, diaphragm electromyography = 56%, respiratory inductive plethysmography = 53%, oronasal thermal device = 44%, and transthoracic impedance = 33%. Apnea definitions were heterogeneous, using variable durations of breathing cessation (median 10s, IQR 5-20s) and not consistently including the co-occurrence of bradycardias and/or oxygen desaturations (n=48 studies, 33%) of variable durations and severity thresholds (Fig 2).
Conclusion(s): There is significant variability in the clinical methods used to monitor apneas and definitions employed in the current literature, making it difficult to draw robust conclusions. Enhanced methods for monitoring apneas (especially obstructive types) as well as standardized guidelines for defining apneas in preterm infants are urgently needed..jpg)