Neonatal/Infant Resuscitation
Neonatal/Infant Resuscitation 2
321 - Current utilization of cuffed vs. uncuffed endotracheal tubes amongst Near4Neos NICUs
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 321
Publication Number: 321.348
Publication Number: 321.348
Jennifer Rumpel, University of Arkansas for Medical Sciences College of Medicine, little rock, AR, United States; Corey Nagel, University of Arkansas for Medical Sciences, Little Rock, AR, United States; Sydney Rogers, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Sara E.. Peeples, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Richard W. Hall, University of Arkansas for Medical Sciences, Little Rock, AR, United States; Ayman Abou Mehrem, University of Calgary, Calgary, AB, Canada; David Tingay, Murdoch Children's Research Institute, Parkville, Victoria, Australia; Kate Hodgson, Royal Women’s Hospital, Parkville, Victoria, Australia; Joyce O Shea, The Royal Hospital for Children, Glasgow, Glasgow, Scotland, United Kingdom; Nicole Pouppirt, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Lindsay Johnston, Yale School of Medicine, New Haven, CT, United States; Mihai Puia-Dumitrescu, University of Washington School of Medicine, Seattle, WA, United States; Tyler Kenneth. Hartman, Dartmouth Hitchcock Medical Center, Lebanon, NH, United States; Quek Bin Huey, KK Women's and Children's Hospital, Singapore, N/A, Singapore; Kristen Glass, Pennsylvania State University College of Medicine, Hershey, PA, United States; Philipp Jung, Universityhospital Schleswig-Holstein, Luebeck, Schleswig-Holstein, Germany; Stephen DeMeo, WakeMed Children's Hospital WakeMed Health and Hospitals, Raleigh, NC, United States; Taylor Sawyer, University of Washington School of Medicine, Seattle, WA, United States; Shilpi Chabra, University of Washington School of Medicine, Seattle, WA, United States; James Barry, University of Colorado School of Medicine, centennial, CO, United States; Rebecca Shay, University of Colorado School of Medicine, Denver, CO, United States; Jae H.. Kim, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Jennifer Unrau, University of Calgary, Calgary, AB, Canada; Ahmed Moussa, Universite de Montreal, Faculty of Medicine, Westmount, PQ, Canada; Michael Wagner, Medical University of Vienna, Vienna, Wien, Austria; Akira Nishisaki, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Elizabeth Foglia, Perelman School of Medicine at the University of Pennsylvania, Swarthmore, PA, United States

Jennifer Rumpel, MD
Neonatologist
University of Arkansas for Medical Sciences College of Medicine
little rock, Arkansas, United States
Presenting Author(s)
Background: Uncuffed endotracheal tubes (ETTs) are the standard of care for intubation in neonates. Cuffed ETTs are used with caution due to historical data regarding complications, including acquired subglottic stenosis, associated with cuffed ETTs. However, recent evidence, primarily from anesthesia, suggests that cuffed ETTs may be safe to use in some neonates.
Objective: We hypothesized that cuffed ETT use does not increase the risk of the composite outcome of tracheal injury (subglottic stenosis or tracheal surgical intervention including tracheal dilation or reconstruction).
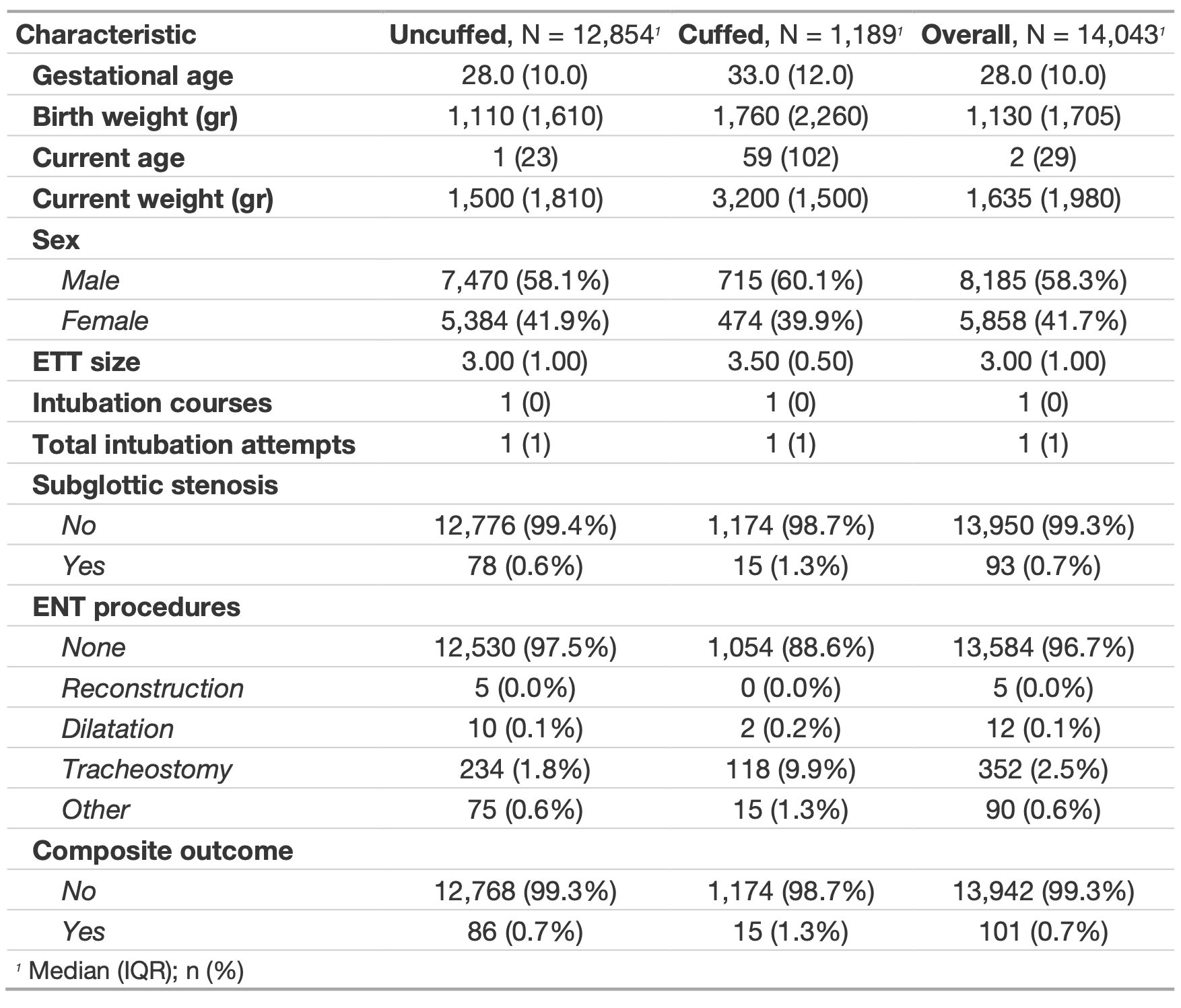
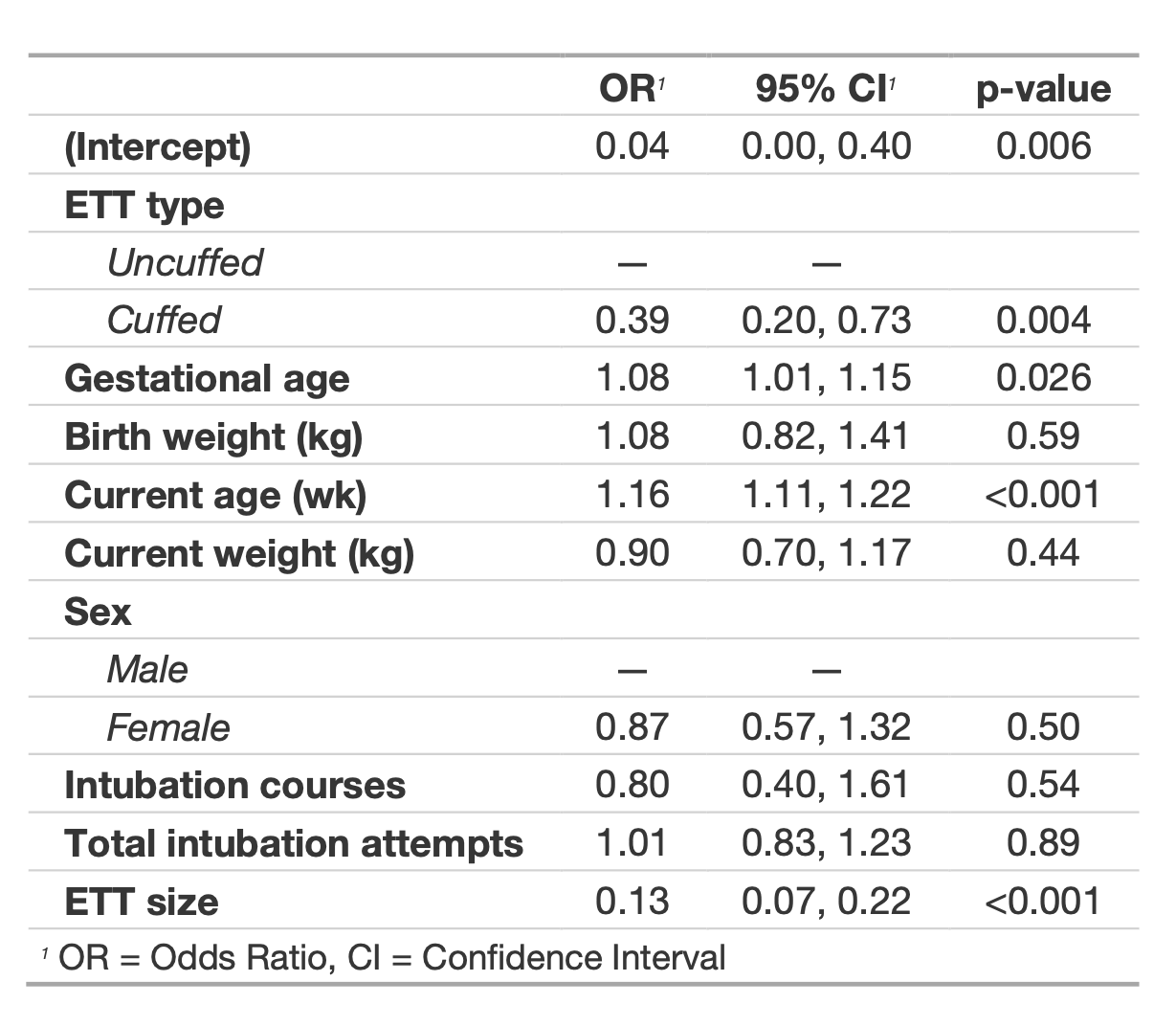
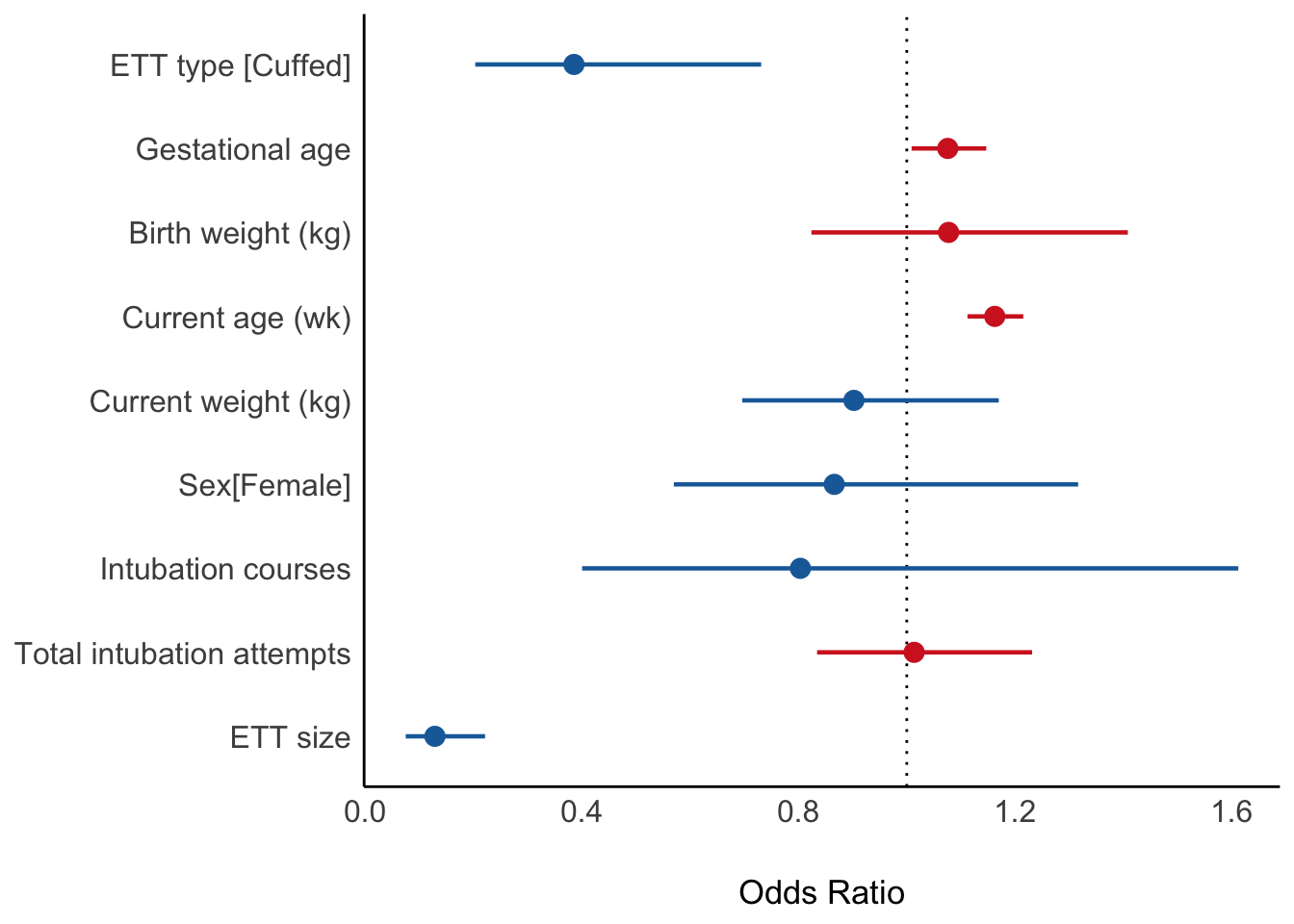
Design/Methods: Retrospective data were collected from 21 international neonatal intensive care units (NICUs) that participate in the Near4Neos collaborative from 2014-2022. An intubation encounter refers to the complete sequence of events leading to the placement of an advanced airway (i.e., cuffed vs uncuffed ETT). The frequency of successfully placed cuffed vs uncuffed ETT for all encounters was compared. Demographics and clinical outcomes for neonates exposed to a cuffed ETT vs uncuffed ETT were described. A mixed effect logistic regression model examined the exposure to a cuffed ETT on the development of the primary composite outcome for tracheal injury (i.e., subglottic stenosis, tracheal dilation or tracheal reconstruction). Potential confounders included in the model were birthweight, weight at the time of intubation, gestational age, postnatal age (days), gender, ETT size, number of previous intubation encounters, and the total number of intubation attempts over all encounters.
Results: 14,043 (number of encounters) were assessed and the frequency of successfully placed cuffed ETT was 1,189 (8.5%) vs 12,854 (91.5%) uncuffed ETT. The most frequent indication for intubation with a cuffed ETT was ventilation failure (20.2%). The median (IQR) gestational age and weight at the time of intubation with a cuffed ETT were 33.0 (12.0) weeks and 1,760 (2,260) grams, respectively. 15 (1.3%) neonates developed the primary composite outcome in the cuffed ETT group vs 86 (0.7%) in the group not exposed to a cuffed ETT. In the fully adjusted model, exposure to a cuffed ETT was associated with decreased odds (aOR:0.39; 95% CI:0.20-0.73) of the composite outcome for tracheal injury. Increased postnatal age and ETT size were identified as risk factors for the composite primary outcome.
Conclusion(s): Cuffed ETTs may be safe for use in neonates in appropriate patients. Future research should examine the contribution of the risk factors of post-natal age and ETT size to the development of the composite outcome of tracheal injury.