Neonatal General
Neonatal General 7: NICU Practices 1
175 - Implementing a Framework for Psychological Safety in the NICU
Publication Number: 175.331

Luke T. Viehl, MD (he/him/his)
Newborn Medicine Fellow
Washington University in St. Louis School of Medicine
Saint Louis, Missouri, United States
Presenting Author(s)
Background: Psychological safety (PS) is the belief that one will not be punished or humiliated for speaking up with ideas, questions, concerns, or mistakes and the team is safe for interpersonal risk taking. Teams with high PS are more likely to share ideas, learn from mistakes, quickly adapt, innovate, and out-perform. PS is relevant to healthcare teams because they work in highly complex, dynamic, and error-prone work environments that require them to interdependently coordinate safe patient care. However, most teams lack high PS, and this includes NICU care teams. At baseline, > 50% of our team members do not feel safe to speak-up on issues and share feedback. We piloted an education program that included specific evidence-based strategies and a self-assessment to cultivate PS.
Objective: To increase our team member PS as determined by quarterly surveys through an intentional 4-week program.
Design/Methods:
Our PS education program included a 90 min interactive didactic session utilizing real life scenarios, evidence-based interventions, and a weekly self-assessment tool. The PS strategies focused on how to: a) build trusting relationships among team members b) emphasize the purpose and value each person contributes c) use humility and curiosity to invite participation to ensure all team members feel valued and d) respond productively to input from all team members.
A NICU triad leadership team (MD, nursing director, and family partner) led 4 sessions in one of 3 areas in our 150-bed level IV NICU. Following the education, participants completed the PS self-assessment tool weekly and committed to practice and improve upon one specific evidence-based PS behavior. Learnings were shared with the triad leaders who rounded for 4 consecutive weeks to assimilate PS behaviors and tools into each participant’s standard work. A 3-question survey was administered quarterly to monitor progress.
Results:
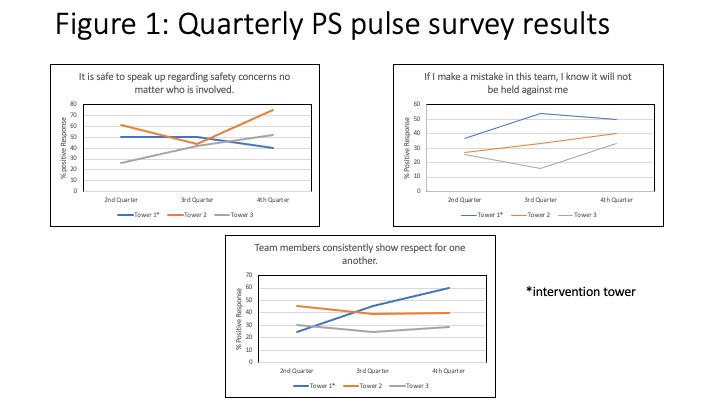
Since March 2022, 62 staff members have completed the intervention program. At baseline, 52% felt that mistakes were held against them personally or professionally, 39% believed they were not consistently shown respect and 45% of respondents did not feel safe to speak up and/or share feedback.
Team members showing consistent respect for one another has increased step-wise in our intervention tower from 25% to 60% (Fig 1).
Conclusion(s):
This is promising data as proof of concept of an educational program with specific evidence-based strategies to improve PS in the NICU. We plan to spread this work to the entire NICU and speculate that an increase in PS will lead to high performing teams and improved patient safety.