Neonatal Follow-up
NICU Follow Up and Neurodevelopment 4: Very Long and Long Term Follow-Up
136 - Behavioral, social and emotional difficulties among five-year-old children born very preterm: results from a European cohort
Publication Number: 136.362
- JZ
Jennifer Zeitlin, DSc., MA (she/her/hers)
Senior Research Director
Inserm
Paris, Ile-de-France, France
Presenting Author(s)
Background:
Children born very preterm (VPT, < 32 weeks’ gestational age [GA]) have higher risk of behavioral, social, and emotional difficulties (BSED) than term-born children. These are an important concern, as they can persist into adulthood and may have a negative impact on quality of life and learning and performance at school.
Objective: To determine the prevalence and perinatal and sociodemographic factors associated with BSED at five years among VPT-born children.
Design/Methods:
Children born VPT in 2011-12 in 19 regions in 11 European countries were included in the analysis (n=3,501). Perinatal characteristics were abstracted from obstetrical and neonatal records. Information on family characteristics and child health was collected using parent questionnaires when the child was five years of age, including the Strengths and Difficulties Questionnaire (SDQ) to assess BSED. The SDQ total score was computed (range 0-40; higher scores indicate greater difficulties). BSED was defined as an SDQ total score ≥80th percentile using UK norms. Logistic regressions adjusted for country were performed to analyze the associations between perinatal and sociodemographic factors and BSED.
Results:
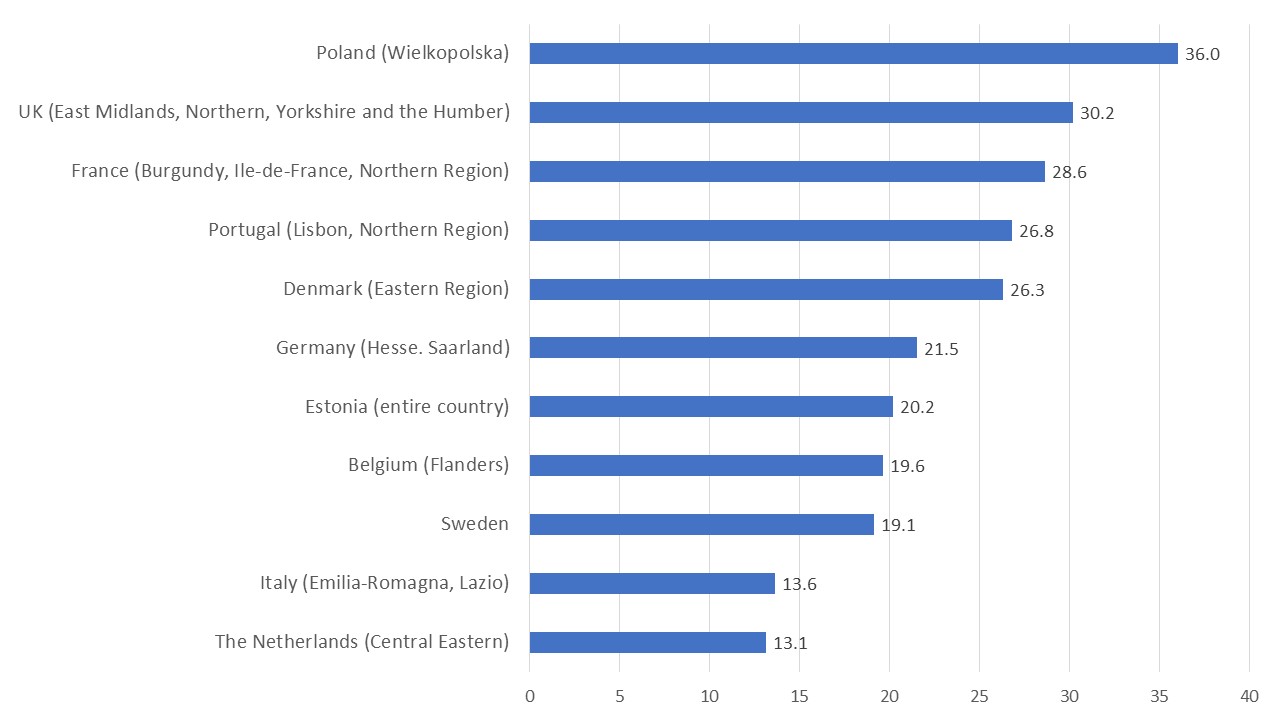
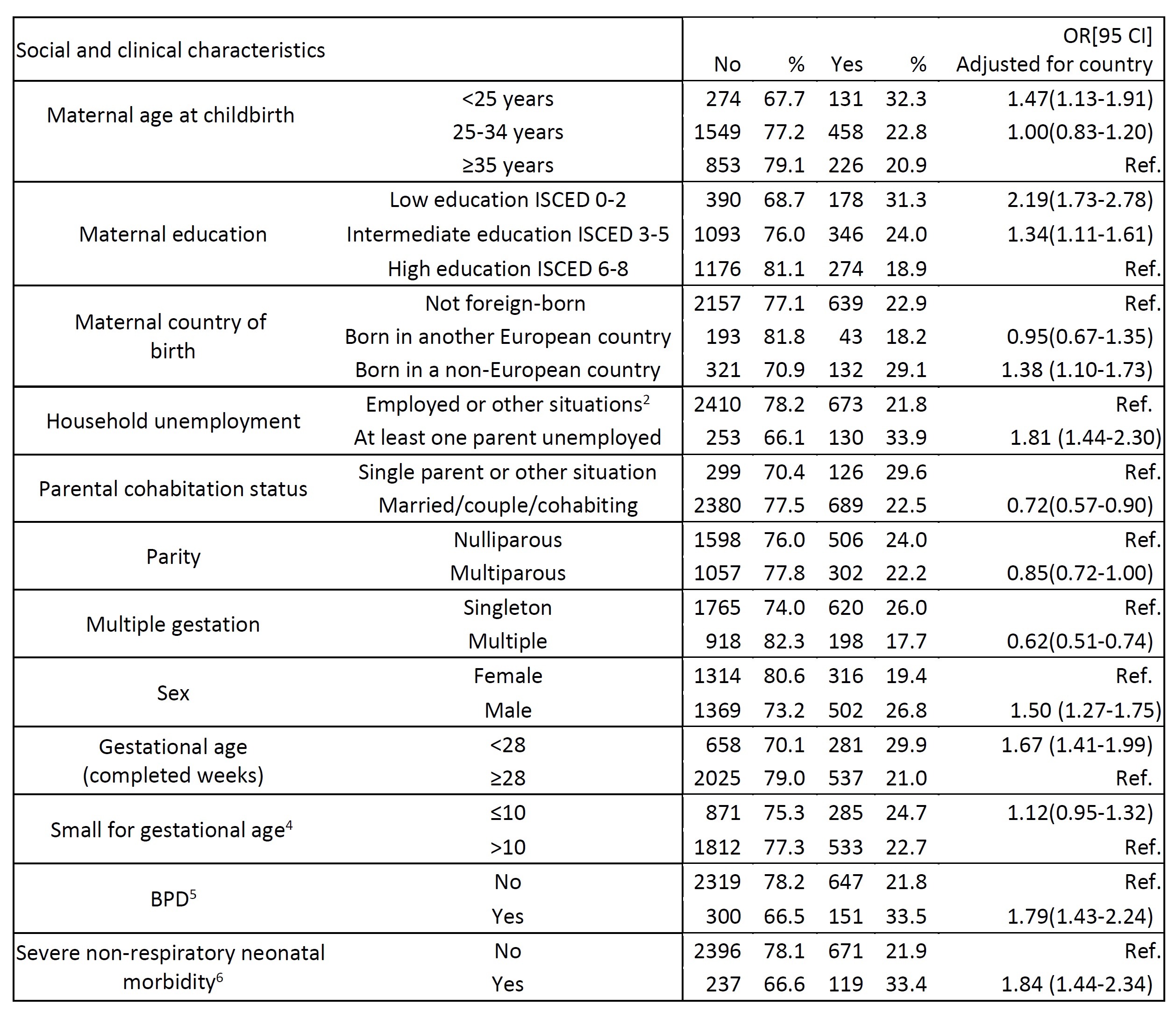
Mean GA at birth was 28.8 (SD=2.0) weeks and mean birthweight was 1238.9 (SD=369.2) grams. Overall, 23.3% of children had BSED, ranging from 13.1% in The Netherlands and 36% in Poland (Figure 1). Having BSED was associated with younger maternal age [< 25 years; OR; 95% CI 1.47; 1.13–1.91], low or intermediate maternal education [2.19; 1.73–2.78 and 1.34; 1.11-1.61, respectively], mother born in a non-European country [1.38; 1.10–1.73], having at least one parent unemployed [2.82; 1.42–5.60], being male [1.50; 1.27–1.75], born < 28 weeks of gestation [1.67; 1.41–1.99], having congenital anomalies [1.50; 1.14–1.96], bronchopulmonary dysplasia [1.79; 1.43–2.24] and non-respiratory severe neonatal morbidity, defined as a composite measure of cystic periventricular leukomalacia, intraventricular hemorrhage grades III and IV, necrotizing enterocolitis that required surgery or peritoneal drainage and retinopathy of prematurity ≥stage 3, [1.84; 1.44–2.34]. Children of married/couple/cohabiting/, or multiparous women and of multiple gestation were less likely to have BSED (Table 1).
Conclusion(s): Multiple social and clinical factors raise risks of BSED. Screening for BSED in early childhood may identify children at greatest risk for whom early intervention may be warranted. Large differences in the prevalence of BSED between countries requires further study.