Nephrology: Transplant
Nephrology 4: Transplant
31 - Comprehensive urologic evaluation before pediatric kidney transplantation improves graft outcomes
Publication Number: 31.349
- EB
Eric Benz, MD (he/him/his)
Assistant Professor of Pediatrics
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background:
While congenital anomalies of the kidney and urinary tract (CAKUT) are the most common cause of ESKD in children, pre-transplant urologic evaluation is often limited to those patients with a urologic history. Post-transplant course, in all patients (regardless of etiology of ESKD) may be complicated by upper/lower GU tract dysfunction impacting graft and patient health. Early identification of children at risk for urologic dysfunction during the transplant process may help improve long term graft and patient outcomes for children with ESKD regardless of etiology.
Objective:
We hypothesize that preemptive, comprehensive urologic evaluation (CUE) in all children with ESKD will improve graft/patient outcomes in pediatric patients undergoing kidney transplantation.
Design/Methods:
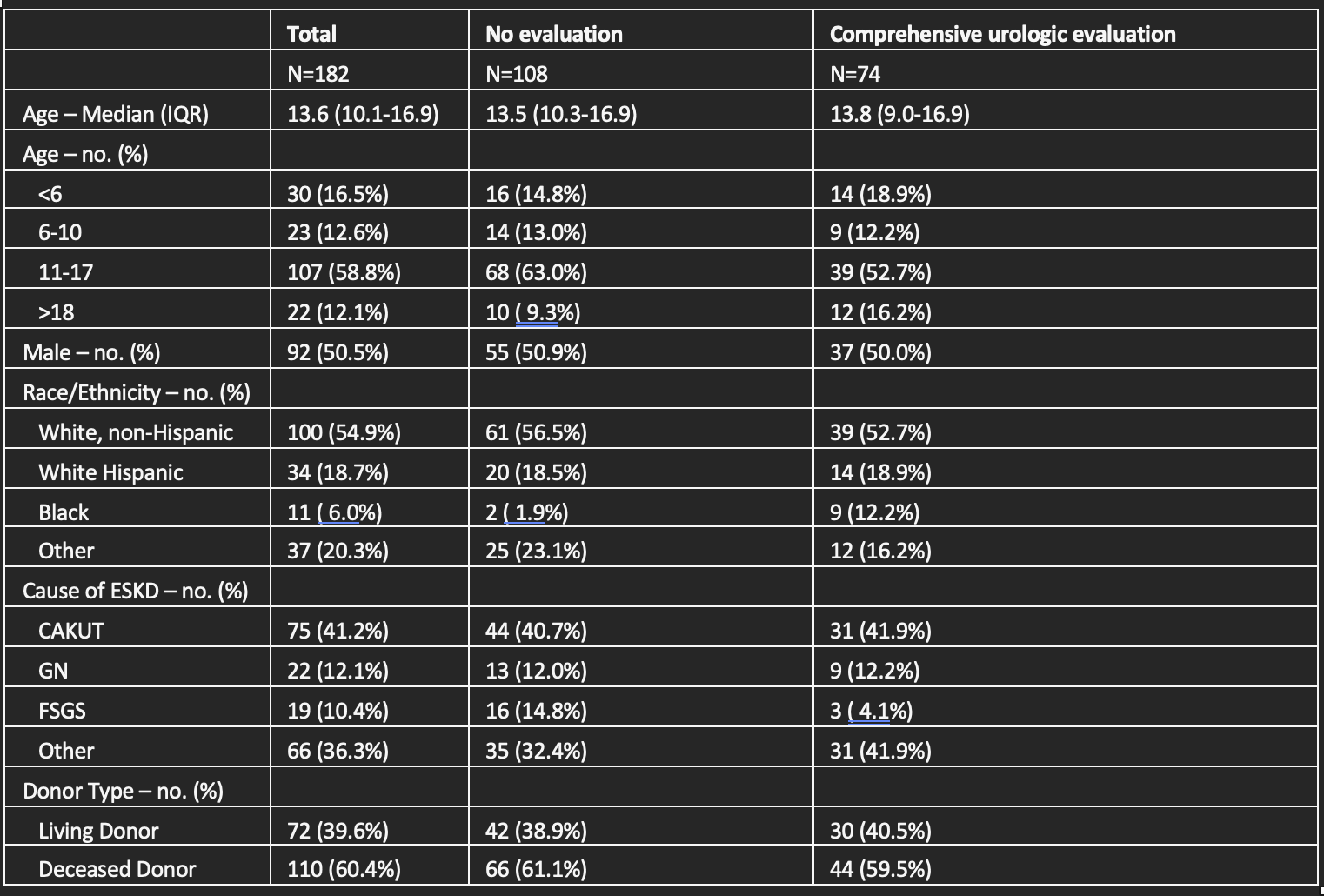
We implemented a CUE (including imaging, lower and upper tract evaluation, and development of individualized treatment plans) in all children undergoing kidney transplant evaluation, regardless of diagnosis of ESKD. We performed a single center, retrospective cohort study of pediatric (< 21 years old) kidney transplant recipients from 2014 – 2022; pre-CUE (2014-2018) outcomes were compared to post-CUE (2019-2022) outcomes. Relevant recipient demographic and outcome data were collected. Multivariable logistic regression was performed to examine associations between receiving a CUE and recipient graft outcomes.
Results:
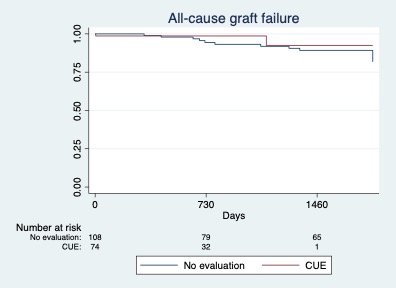
182 kidney transplant recipients were included in our cohort with similar age, sex, and race/ethnicity (Table 1). The most common cause of ESKD was CAKUT (41%); prevalence was similar in pre- and post-CUE cohorts. 12 graft losses were observed in the pre-CUE cohort (5 with CAKUT), with only 2 graft losses (non-CAKUT) in the post-CUE cohort. Our multivariable logistic regression showed an increased odds of graft loss, regardless of diagnosis of ESKD, (OR 0.2 [0.4-0.99], p< 0.05) for patients who did not undergo a CUE. There was not a significant association with rejection episodes for patients not undergoing a CUE.
Conclusion(s):
Including CUE as part of routine kidney transplantation evaluation, regardless of the cause of ESKD, improves graft outcomes. Further evaluation of the impact of individualized urologic treatment plans on outcomes for pediatric patients undergoing kidney transplantation is warranted.