Neonatal General
Neonatal General 8: NICU Practices 2
180 - Heart Rate Variability Correlates with Intraventricular Hemorrhage or Mortality in Preterm Infants Early in Life
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 180
Publication Number: 180.332
Publication Number: 180.332
Michael Scahill, Stanford University School of Medicine, Walnut Creek, CA, United States; Eric D. Helfenbein, Philips Healthcare, Sunnyvale, CA, United States; Molly F.. Lazarus, Stanford University School of Medicine, Menlo Park, CA, United States; Katherine Travis, Stanford University School of Medicine, Palo Alto, CA, United States; Valerie Y. Chock, Stanford University School of Medicine, Sunnyvale, CA, United States; Melissa Scala, Stanford University School of Medicine, Palo Alto, CA, United States

Michael Scahill, MD, MBA (he/him/his)
Clinical Assistant Professor
Stanford University School of Medicine
Walnut Creek, California, United States
Presenting Author(s)
Background: The heart rate variability (HRV) measure sample entropy has proved valuable for diagnosis and risk prediction of neonatal sepsis. Neonatal intraventricular hemorrhage (IVH), associated with poor neurodevelopmental outcome and death in preterm infants, is challenging to predict or diagnose in a timely fashion. As HRV reflects an interplay between the autonomic nervous and cardiac systems, we aimed to explore associations between sample entropy in the first week of life and IVH or mortality.
Objective: To explore sample entropy as an early predictor of IVH and mortality in preterm infants
Design/Methods: Infants were < 32 weeks gestational age (GA), inborn and admitted to a Level IV neonatal intensive care unit from July 2017 through December 2021. Clinical outcomes included mortality prior to hospital discharge and IVH as determined by routine head ultrasound on day of life 7-10. Philips PIC iX Data Warehouse Connect provided continuous ECG monitoring at 500 Hz. The PhysioNet Cardiovascular Signal Toolbox calculated HRV using 5-minute windows stepped by 30 seconds. Logistic regressions evaluated sample entropy as either birth-to-censor point average or 8hr moving average at different hours of life (HOL) censor time points. Models controlled for GA, birthweight, sex, 5-minute Apgar, average heartbeat interval and low frequency:high frequency HRV ratio.
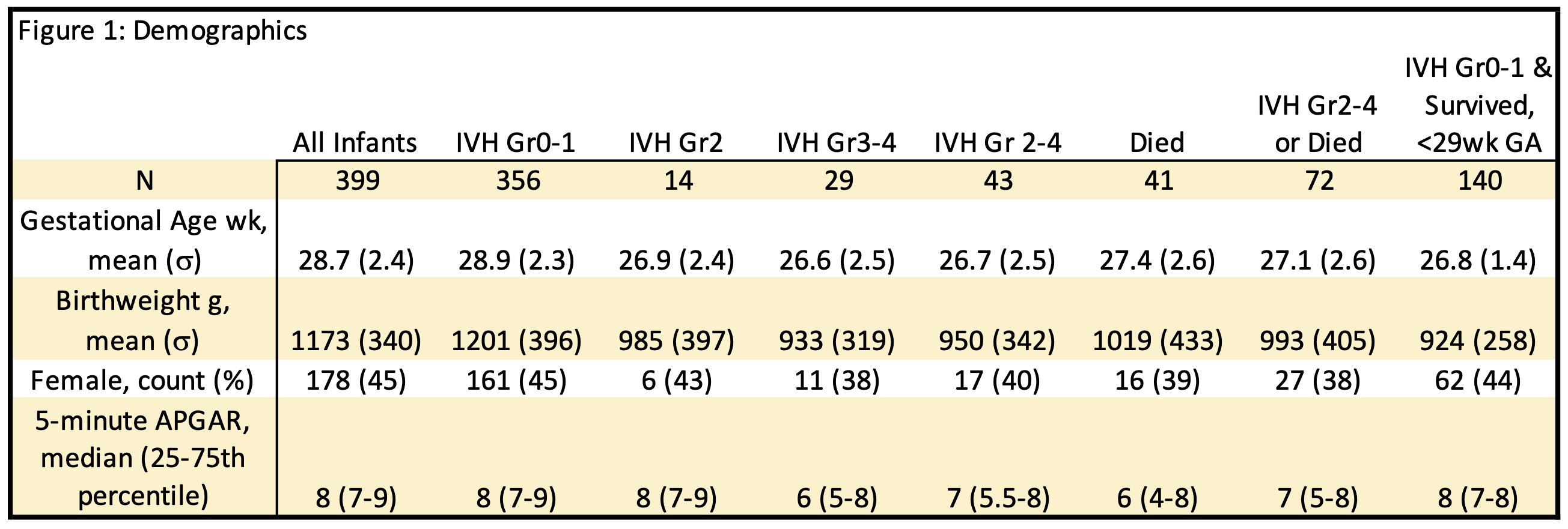
Results: A total of 399 infants with mean GA 28.7 wk were studied (Fig 1). By 24 HOL, sample entropy was higher among infants with IVH grades (Gr) 2-4, mortality and the composite thereof relative to controls. This difference was greater among high risk, GA < 29 wk infants (Fig 2). Regressions showed moving average was a significant predictor by 24 HOL for IVH and by 18 HOL for mortality or the composite outcome. Birth-to-censor point average predicted outcomes starting at 48-72 HOL and continued through the first week of life (Fig 3). Among known predictors, lower GA was associated with all outcomes and lower Apgar with mortality and the composite. Other coefficients did not reach significance.
Conclusion(s): A detectable rise in sample entropy may be an early predictor of mortality or IVH in preterm infants. More research is needed to explore how such an HRV analysis may be used to enable clinicians to anticipate adverse outcomes in preterm infants.
.png)
.png)
