Environmental Health
Environmental Health
613 - Odds of ICU Admission for Asthma Associated with Fine Particulate Matter Air Pollution Among Pediatric Population
Publication Number: 613.313

Diane Peng, MD (she/her/hers)
Fellow, Pediatric Critical Care
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: Air pollution is associated with adverse health outcomes, including intensive care unit (ICU) admission and mortality in adults. However, the impact on children is not as clearly understood.
Objective: Measure the association of total, smoke, and non-smoke fine particulate matter (PM2.5) air pollution and odds of (1) all-cause ICU admission and (2) ICU admission for asthma in the pediatric population.
Design/Methods: We performed a time-stratified case-crossover study of ICU admissions among 42 US children’s hospitals from 2010-2020. Only hospitalizations through the emergency room with ICU admission in the first 7 days were included. PM2.5 levels were derived from the Environmental Protection Agency’s Air Quality System monitors and the National Oceanic and Atmospheric Administration's Hazard Mapping System smoke plumes for each hospital zip code. Patient and hospitalization characteristics were obtained from clinical and billing data. We used quasi-binomial regression models with distributed-lagged effects averaged from days 0-5 to estimate the odds of ICU admission, controlling for natural splines of temperature, relative humidity, and co-pollutants of PM10, NO3, and O3 at 10 km buffer zones.
Results:
Over the study period, 181,222 ICU admissions met criteria for inclusion (Table 1). Respiratory conditions were the most common reason for admission, 27% of which had a primary diagnosis of asthma. For all-cause ICU admissions, we found a nonsignificant decreased odds of admission by 0.08% (95% CI: -0.19, 0.04 p=0.18) for each 1 µg/m3 increase in total PM2.5. Separating PM2.5 into smoke and non-smoke components also yielded nonsignificant decreased odds of all-cause admission by 0.31% (95% CI: -0.62, 0.00 p=0.05) and 0.05% (95% CI: -0.18, 0.08 p=0.63) for each 1 µg/m3 increase in smoke and non-smoke PM2.5, respectively.
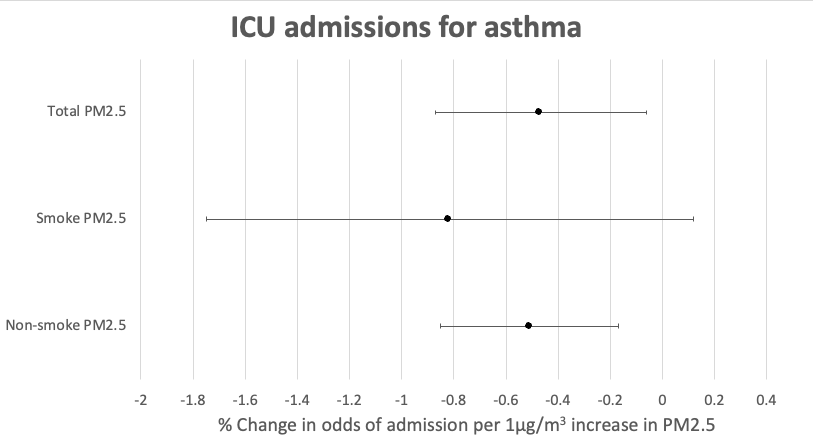
For ICU admissions for asthma, we found a significant decreased odds of admission by 0.51% (95% CI: -0.85, -0.17 p=0.003) for each 1 µg/m3 increase in total PM2.5. Separating PM2.5 into smoke and non-smoke components yielded nonsignificant decreased odds of admission by 0.82% (95% CI: -1.75, 0.12 p=0.10) and significant decreased odds of admission by 0.47% (95% CI: -0.87, -0.06 p=0.02) for each 1 µg/m3 increase in smoke and non-smoke PM2.5, respectively.
Conclusion(s): This pediatric study shows higher air pollution levels were not associated with increased odds of ICU admission, yet were associated with decreased odds for asthma admission. This unexpected finding may be due to heightened awareness of unhealthy air quality leading to behavioral change but needs further exploration..png)
.png)