Neonatal Follow-up
NICU Follow Up and Neurodevelopment 5: Impact of Parents and Social Determinants of Health
151 - A Transition Home Program during COVID-19 and the association between maternal mental health with ER visit and rehospitalization rates among NICU graduates
Publication Number: 151.363
- JM
Julia P. Mayne, MD MS (she/her/hers)
Assistant Professor
Women & Infants Hospital of Rhode Island
Providence, Rhode Island, United States
Presenting Author(s)
Background: Infants in the neonatal intensive care unit (NICU) are at increased risk of rehospitalization upon discharge. Public insurance and maternal mental health problems further increase this risk. The COVID-19 pandemic was associated with increased mental health problems including anxiety and depression. A transition home program for publicly insured NICU families has been shown to decrease ER visit and rehospitalization rates after discharge. A comparison between cohorts before and during COVID-19 were explored.
Objective:
To determine the association between mental health problems before and during the COVID-19 pandemic among high-risk mother infant dyads participating in a Transition Home Program with infant ER visit and rehospitalization rates at 30 days and 90 days after NICU discharge.
Design/Methods: A retrospective review of a publicly insured cohort of infants in Women & Infants NICU enrolled in a Transition Home Program between 2017 to 2022 was conducted. Groups were stratified to pre-COVID (January 1, 2017-December 31, 2019) and during COVID (January 1, 2020-November 18, 2022). Group characteristics were compared between periods using t-tests/Wilcoxon tests for continuous variables and chi-square tests for categorical variables. Regression models estimating the effects of maternal health on ER visits and rehospitalization rates were evaluated.
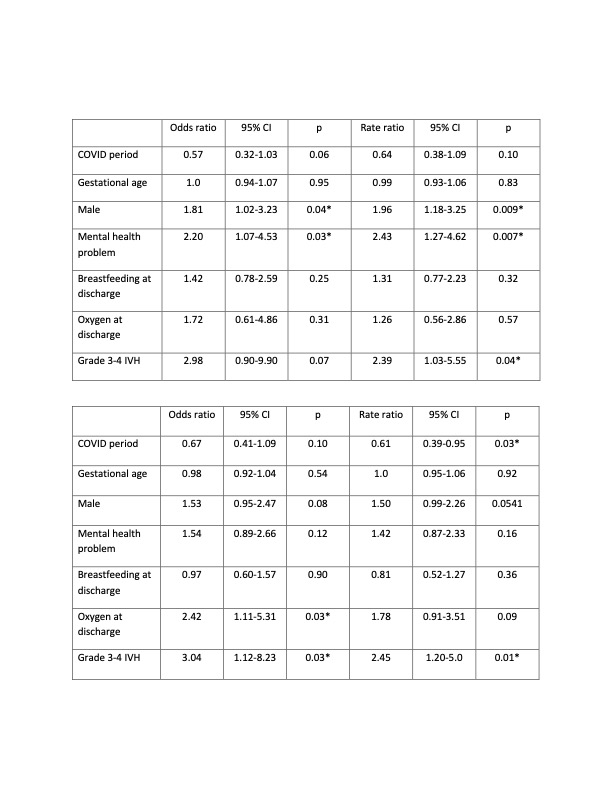
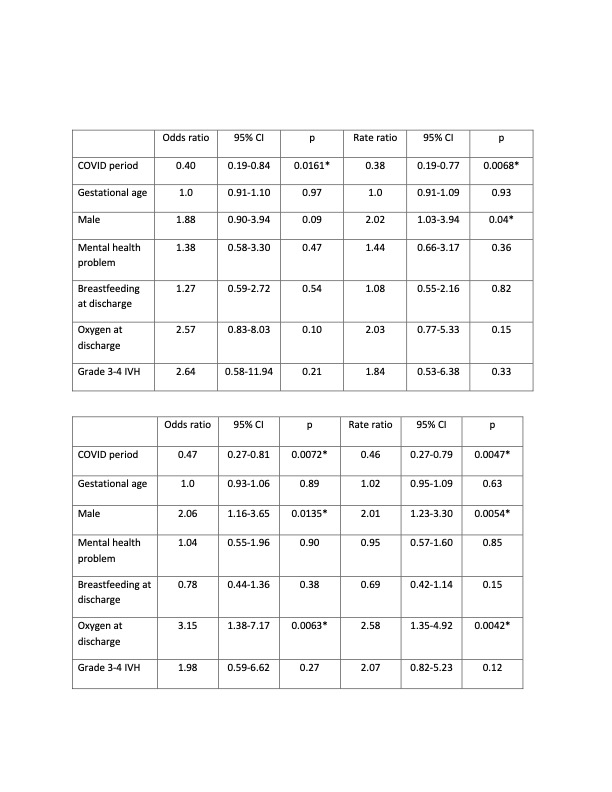
Results: Infants enrolled during COVID-19 were born older and larger than infants enrolled before the pandemic (Table 1). In regression modeling, presence of a maternal mental health problem OR 2.2 (CI 1.07-4.53) and male sex OR 1.81 (1.02-3.23) were associated with an increased risk of ER visits within 30 days of discharge as compared to pre-COVID (Table 2). By 90 days from discharge during COVID-19, oxygen at discharge OR 2.42 (1.11-5.31) and grade 3-4 intraventricular hemorrhage OR 3.04 (1.12-8.23) were associated with an increased risk of ER visits (Table 3). Male sex OR 2.06 (1.16-3.65) and oxygen at discharge OR 3.15 (1.38-7.17) were associated with rehospitalization by 90 days during COVID-19 (Table 5).
Conclusion(s): Infants born to mothers with mental health problems in a Transition Home Program were more likely during the COVID-19 pandemic to have any as well as an increased number of ER visits 30 days after NICU discharge, not rehospitalizations. In contrast, neonatal medical morbidities were associated with greater risk of ER visit and rehospitalization 90 days after discharge. .jpg)