Health Services Research
HSR 3: Social and Medical Complexity
593 - Connecting Immigrant Children with Complex Medical Needs to Health Care
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 593
Publication Number: 593.319
Publication Number: 593.319
Rama Imad, Johns Hopkins School of Medicine, Baltimore, MD, United States; Sarah Polk, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Lorenzo Cruz, Johns Hopkins University School of Medicine, Takoma Park, MD, United States
- RI
Rama Imad, BA (she/her/hers)
Program Coordinator
Johns Hopkins School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: Families of undocumented, low-income children struggle to obtain healthcare. For children with chronic health conditions, healthcare access is critical. In Maryland, un/under-insured, undocumented children with qualifying chronic health conditions can access specialty care and supplies through Children’s Medical Services (CMS). CMS-eligible children often need to enroll in charity care and emergency Medicaid (EMA) to cover additional essential healthcare needs (primary care, emergency care). Hopkins Community Connections (HCC) staff work with families to enroll children in CMS and charity care due to barriers to enrollment encountered by parents of eligible children.
Objective: We aim to inform healthcare policy discussions by describing healthcare experiences of a convenience sample of children of immigrant parents with limited English proficiency who were identified by HCC as medically complex children requiring CMS as well as charity care and EMA. A secondary aim was to understand healthcare costs of the patient sample.
Design/Methods: We present a secondary analysis of administrative and clinical data collected by HCC. We report on data from 34 pediatric patients presumed CMS-eligible based on a qualifying health condition who last received care at our institution between January 2021 and March 2022. We reviewed electronic medical records to understand patients’ healthcare experience as well as billing records to capture financial cost.
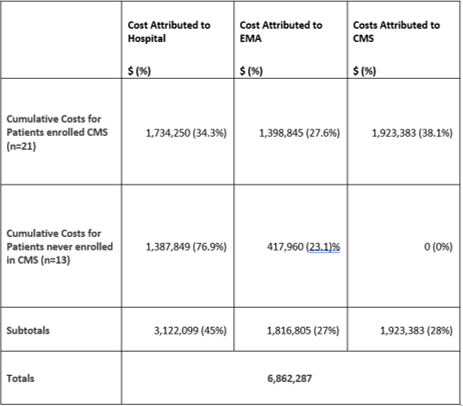
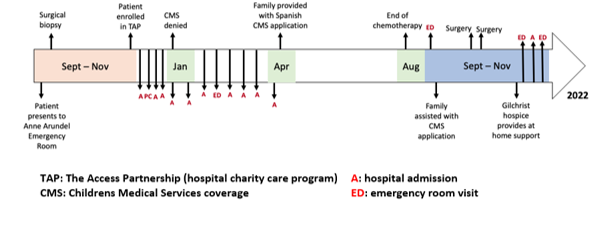
Results: Between 2011 and 2022, 49 CMS-eligible patients presented at our institution. We report on a convenience sample of 34 of these patients. Among them, 29 (85.3%) were Hispanic and 33 (97.1%) spoke Spanish; the average age was 10.4 years old (Table 1). Figure 1 shows the healthcare experience of one patient, including specialty care visits, surgeries, hospital admissions. Amount of time spent applying for but not enrolled in CMS is also shown. The total cost of care for the 34 patients was 6,862,287 (Table 2). Healthcare costs were attributed to CMS ($1,923,383, 28%), charity care ($3,122,099,45%) and EMA ($1,816,805,27%). In the absence of CMS, costs were attributed to charity care.
Conclusion(s): Our findings suggest that as implemented, eligible patients spend a lot of time not enrolled in CMS. CMS enrollment would be greatly facilitated by navigators. In the absence of state-sponsored navigators within the CMS program, hospitals may wish to invest in patient navigation for the benefit of patients and in light of the cost of care of these patients.
.png)