Health Services Research
HSR 3: Social and Medical Complexity
591 - Subspecialty Care Among Patients with Limited English Proficiency: The Perspectives of Spanish-Speaking Families
Publication Number: 591.319

Doris Valenzuela-Araujo, MD (she/her/hers)
Pediatric Resident
Oregon Health & Science University School of Medicine
Portland, Oregon, United States
Presenting Author(s)
Background:
Children in families with LEP face significant health inequalities and healthcare navigation challenges, including confusing subspecialty referral processes and variable accommodations for language needs.
Objective: To understand current care challenges in obtaining subspecialty care among families with LEP and identify opportunities for improvement.
Design/Methods:
A telephone survey with a semi-structured interview was conducted among Spanish-speaking families receiving pediatric gastroenterology care at a large urban academic center. Participants included parents/guardians of children 0-18 years old who identified Spanish as their primary language and had a clinic appointment in June-May2020. Spanish-English proficient research coordinators were trained to standardize the interview process and review responses. Participants were asked about referral reasons, scheduling and interpreter experience, follow-up care, and barriers to care. Data analysis focused on identifying themes in patient perceptions and experiences.
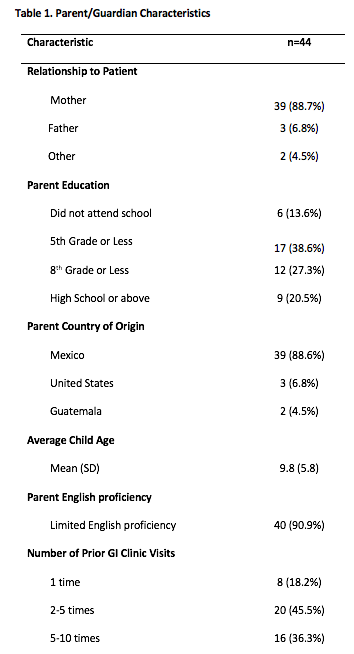
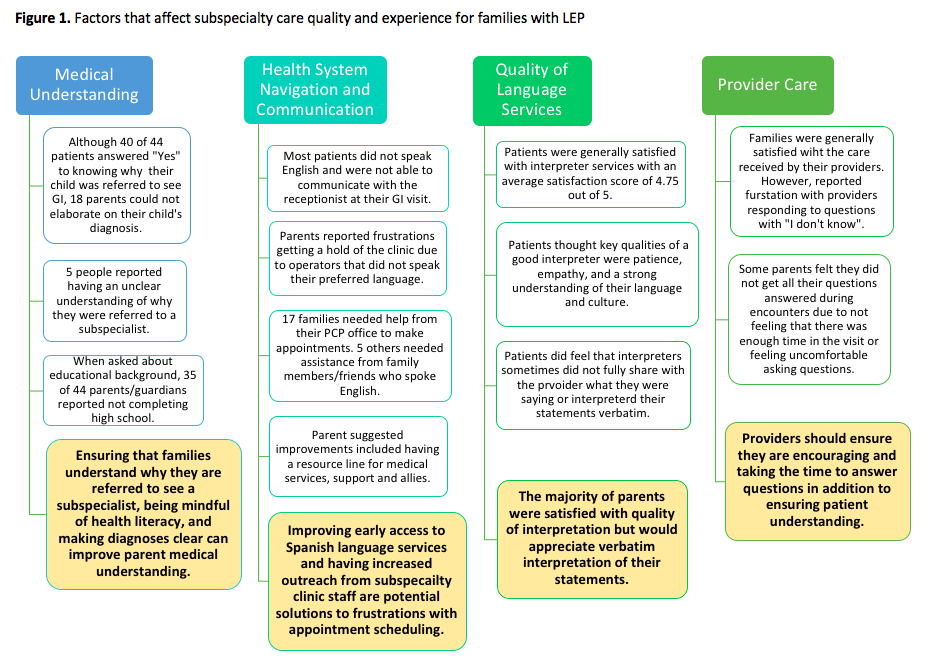
Results: 44 parents/guardians participated in this study, the majority of whom were from Mexico (Table 1). Four main factors were identified as having a key role in affecting the perceived quality of subspecialty care and experience of families with LEP: 1)medical understanding, 2)health system navigation and communication, 3)quality of language services, and 4)provider care (Figure 1). Parents identified pre-visit communication as the most challenging part of attaining specialty care due to multiple hospital-integrated automated calling systems and operators. 57% had to depend on English-proficient individuals (PCP office, family/friends) to schedule their appointment. 46% experienced limited language services, inability to communicate with clinic staff, or being led to confusing voicemails in English, for which some received no callback. Mean visit satisfaction was 3.95/5. Parents emphasized the need for longer appointment times to adequately communicate with their providers, ask questions and understand their child’s diagnosis. Calling and text messages were the preferred methods for clinic communication after visits, not MyChart or emails.
Conclusion(s): Families with LEP continue to face significant challenges in obtaining high-quality subspecialty care. Efforts for improvement should focus on early access to language services, assistance with scheduling appointments, and being mindful of parent health literacy. In addition, extending visit times could improve family comfort in asking questions and subsequently improve medical understanding and adherence to recommendations.