Health Services Research
HSR 3: Social and Medical Complexity
590 - “There is more to good interpretation than just acquiring an interpreter”: Understanding how to improve communication with families with limited English proficiency
Publication Number: 590.319

Doris Valenzuela-Araujo, MD (she/her/hers)
Pediatric Resident
Oregon Health & Science University School of Medicine
Portland, Oregon, United States
Presenting Author(s)
Background:
There continue to be challenges in effective communication and medical understanding for families with limited English proficiency (LEP). Parents with LEP are less likely to have a thorough understanding of their child’s medical condition, understand why their child was referred to a subspecialist, and feel less comfortable asking clarifying questions.
Objective: To understand the challenges to effective communication with LEP families through the perspective of healthcare providers and interpreters and to identify potential interventions.
Design/Methods: This survey study included healthcare providers and interpreters from a large urban academic center. Participants completed an online survey about their experiences caring for LEP families with questions tailored to their role. The provider survey focused on prior training on caring for LEP families, challenges and strengths in using interpreter services, and perceptions on needed improvements. The interpreter survey included perceptions on how doctors can improve their patient communication. Surveys were reviewed to identify themes in characterization of changes needed to improve care for LEP families.
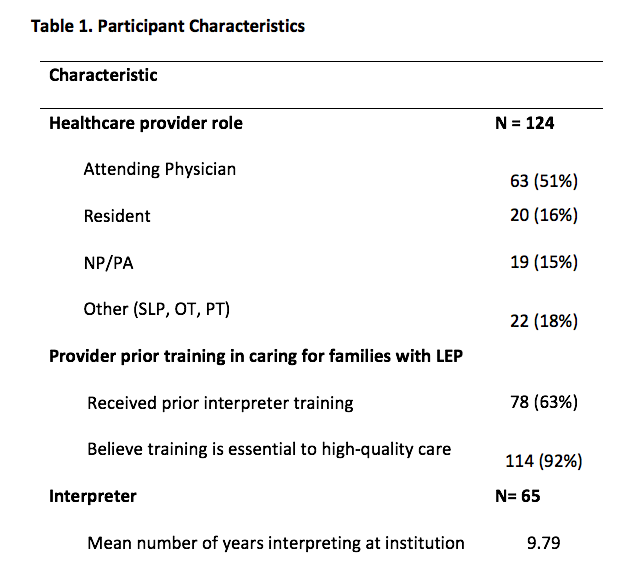
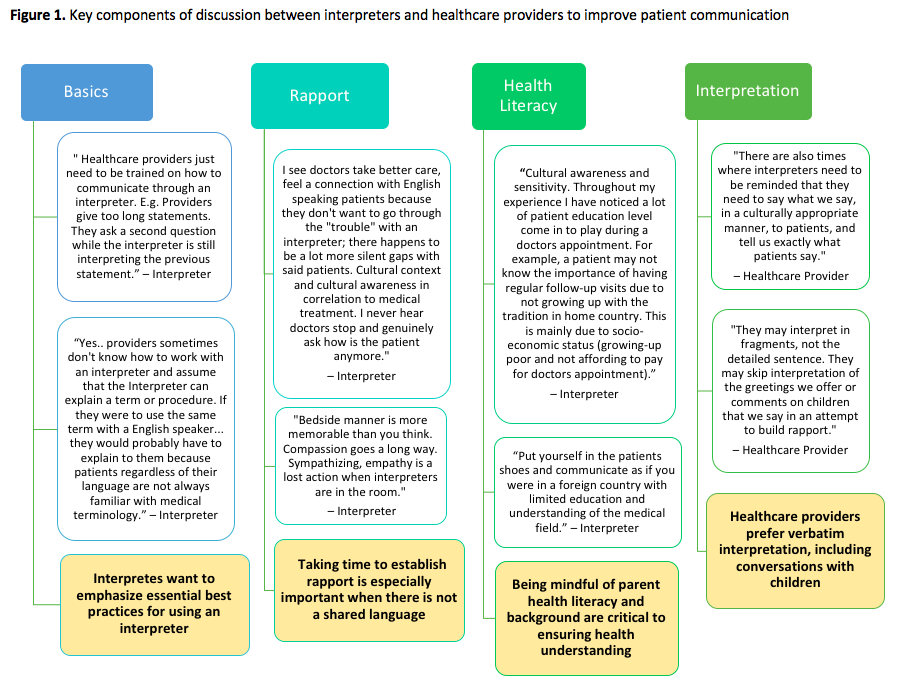
Results: 124 healthcare providers and 65 interpreters participated in this study (Table 1). While 92% of providers felt training on caring for LEP families to was essential to high quality, only 63% of providers had received prior training. 42% of all providers expressed wanting more extensive training. Limited interpreter availability and time constrains were identified as systems-based barriers to effective visit communication. Both interpreters and providers endorsed taking the time to better understand the provider and interpreter roles in conjunction with the family’s needs prior to the visit as being crucial in improving patient medical understanding and visit satisfaction. A pre-visit huddle between providers and interpreters was suggested by both groups as a potential intervention to improve patient communication. Four topics emerged as most critical to include in conversations between these groups; basics, rapport, health literacy, and reviewing expectations of interpreters (Figure 1).
Conclusion(s):
Quality of communication with LEP families is affected by health system and individual-level factors. Addressing hospital logistics to allow for longer appointment times and improved interpreter availability and quality can greatly affect provider satisfaction with the care they provide. In addition, a pre-visit huddle with between interpreters and providers has the potential for improved communication with LEP families.