Health Services Research
HSR 4: National or Novel
604 - Responsiveness and Convergent Validity of a Novel Health-Related Quality of Life Measure in Hospitalized Pediatric Patients and Their Caregivers
Publication Number: 604.32
.jpg)
Holly H. Vo, MD, MPH, MSc, MA (she/her/hers)
Assistant Professor
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background:
Methods: Retrospective analysis of Seattle Children’s Hospital (SCH) PRO Program survey data on patients 0-17 years old (yo) and their caregiver >18 yo (n=308) admitted to SCH between 4/19/2021-10/30/2022. The SCH PRO Program uses a targeted recruitment approach to optimize historically marginalized populations via oversampling based on race, ethnicity, preferred language, and geography. We analyzed data from: (1) patients with both IAR and PedsQLTM 4.0 Generic Core Scales scores on admission; and (2) caregivers of these patients who completed the caregiver IAR survey item, which assesses how their child’s medical concern impacted their own activities and routines on admission and follow-up. Forty-eight percent of patients and caregivers who completed the admission assessment also completed the follow-up assessment 5-7 weeks post-hospital discharge. We assessed responsiveness by calculating improvement scores (difference between admission and follow-up scores). Convergent validity was assessed by Spearman’s correlation coefficients between patient IAR and PedsQLTM total scores. Higher scores reflected worse HRQOL on both measures (1-5 scale).
Background: Patient-Reported Outcome (PRO) measures assessing health-related quality of life (HRQOL) provide valuable information for clinicians and researchers to improve health outcomes. The Impact on Activities & Routines (IAR) is a novel, two-item PRO measure that is concise, easy to understand, and captures both patient and caregiver HRQOL.
Objective:
Objective: Evaluate responsiveness and convergent validity of the IAR measure in the pediatric inpatient setting.
Design/Methods:
Results:
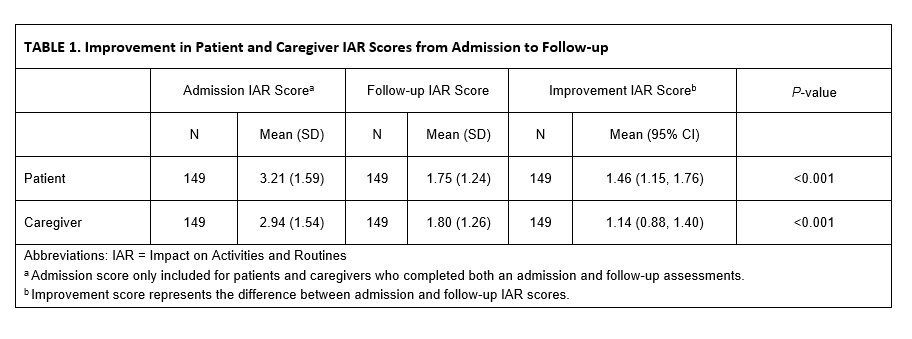
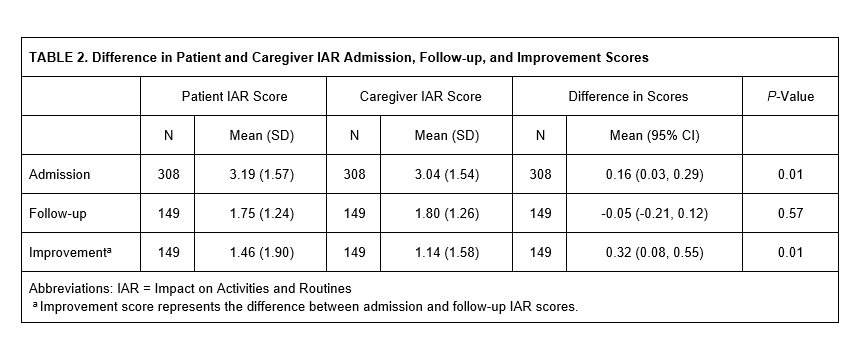
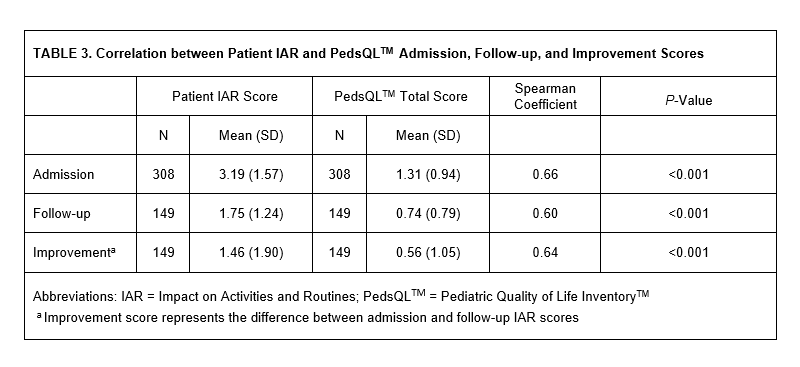
Results: Patient IAR scores on admission was significantly higher than at follow-up (mean (SD): 3.21 (1.59) vs 1.75 (1.24), p< 0.001); mean improvement score was 1.46 [95% CI, 1.15-1.76] (Table 1). Caregiver IAR scores on admission was significantly higher than follow-up (2.94 (1.54) vs 1.80 (1.26), p< 0.001); mean improvement score was 1.14 [95% CI, 0.88-1.40] (Table 1). Compared to caregivers, patients had significantly higher IAR admission and improvement scores (Table 2). Patient IAR scores were strongly correlated with PedsQLTM total admission, follow-up, and improvement scores (Spearman coefficient 0.66, 0.60, and 0.64, respectively, p< 0.001, Table 3).
Conclusion(s):
Conclusions: The IAR measure demonstrates responsiveness to clinical interventions and convergent validity with a well-known HRQOL measure in hospitalized pediatric patients. The IAR may be a useful and efficient PRO measure for assessing both patient and caregiver HRQOL for clinical effectiveness research.