Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 6
659 - Investigating Clinicians' Perspectives on Trust, Communication, and Health Disparities within a Pediatric Emergency Department
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 659
Publication Number: 659.317
Publication Number: 659.317
Eden Efrem, Children's National Hospital, Silver Spring, MD, United States; Anaja Pinnock-Williams, Children's National Health System, Wheaton, MD, United States; Marcus E. Russell, George Washington University School of Medicine and Health Sciences, Washington, DC, United States; Monika Lemke, Children's National Health System, Westminster, MD, United States; Monika Goyal, Children's National Health System, Washington, DC, United States

Eden Efrem, BA (she/her/hers)
Clinical Research Assistant
Children's National Hospital
Silver Spring, Maryland, United States
Presenting Author(s)
Background: Quality of care differs by patient race and ethnicity in pediatric emergency departments (PED). Understanding clinicians’ perspectives on the factors contributing to health inequities could provide further insight into how to mitigate these issues.
Objective: To understand clinicians’ perspectives on the contributors to racial and ethnic inequities in a PED.
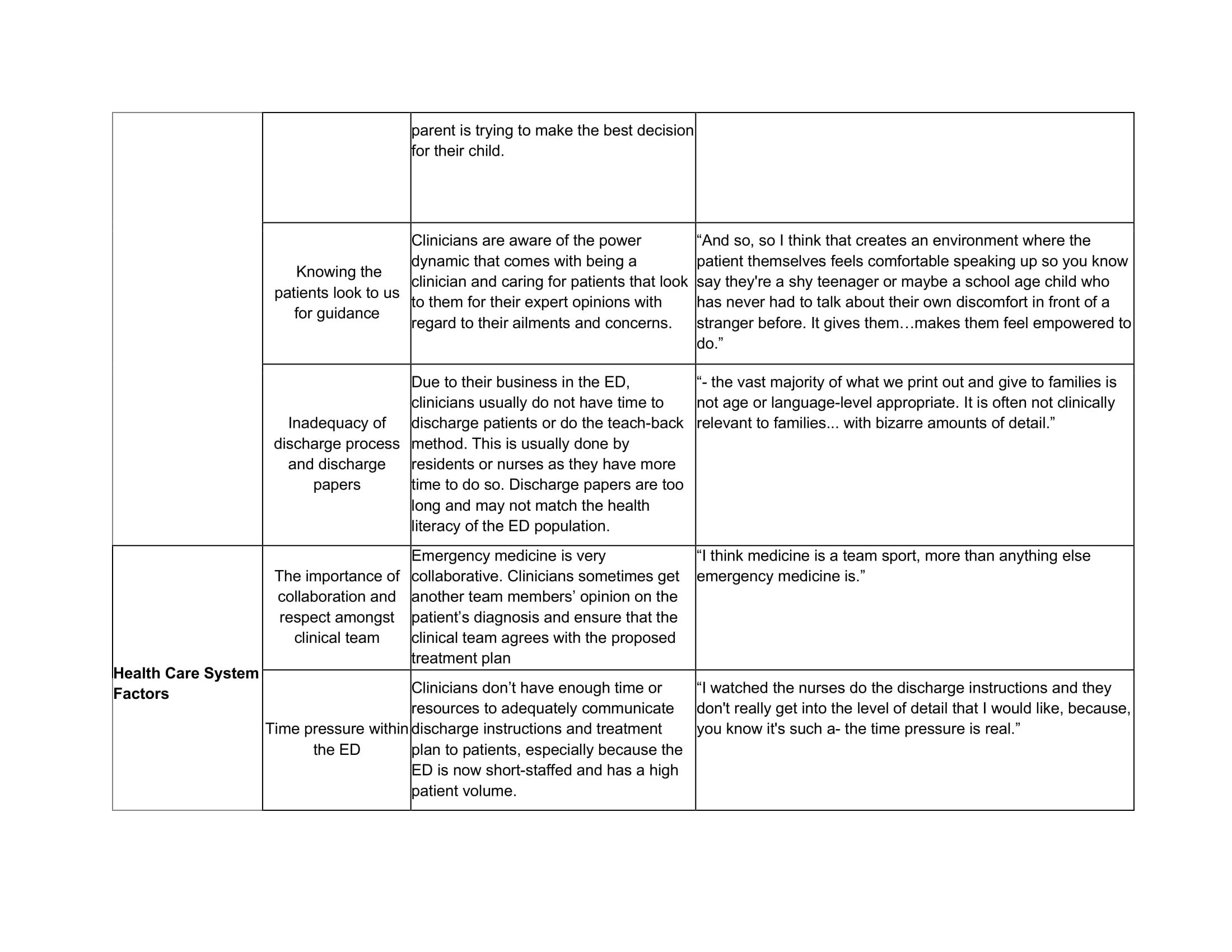
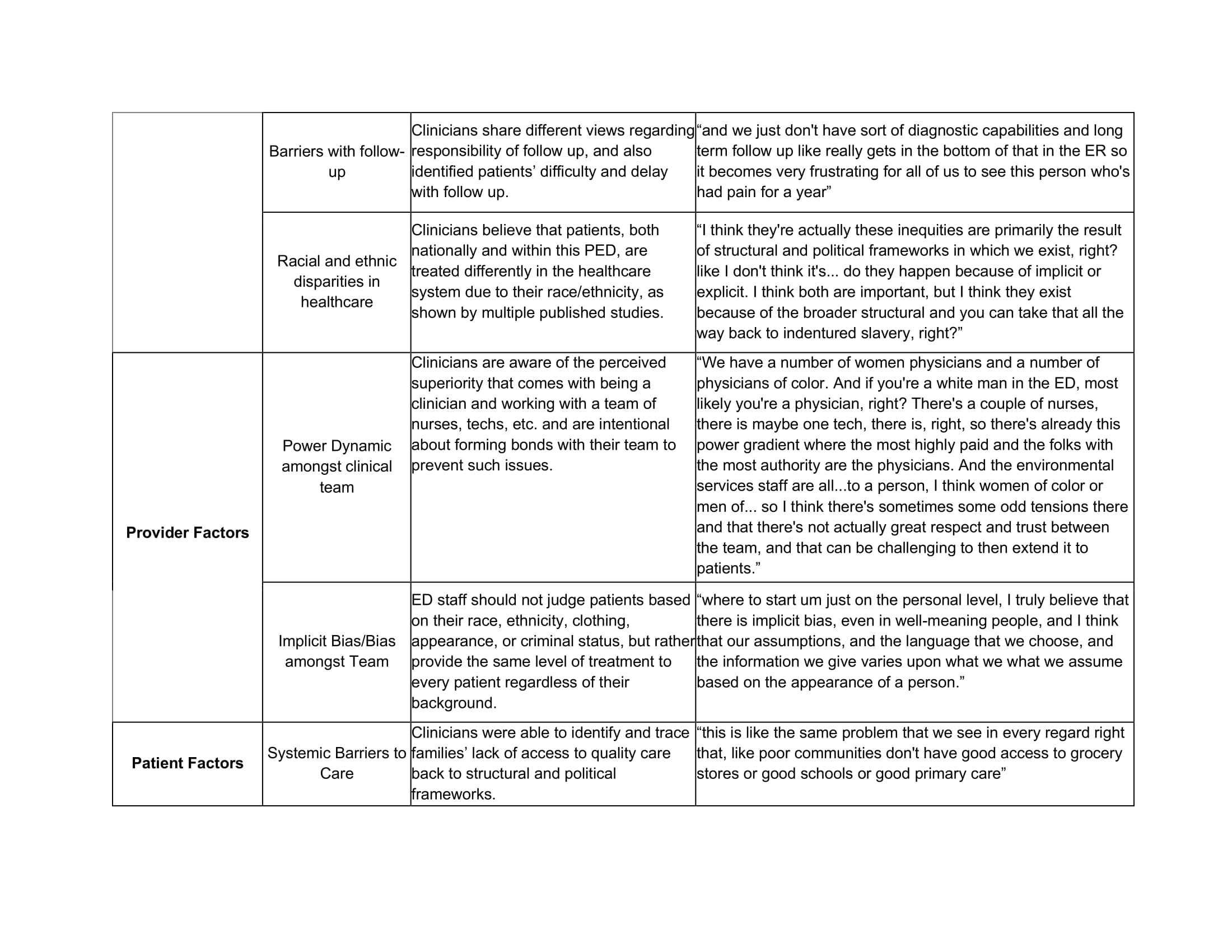
Design/Methods: One-on-one semi-structured interviews with PED clinicians were conducted as part of a pilot study assessing racial and ethnic inequities in pain management from July 2022 to September 2022. Eligible clinicians included pediatric emergency medicine (PEM) attendings, general pediatricians, PEM fellows, physician assistants, and nurse practitioners who had treated ≥1 patient with a chief complaint of acute abdominal pain or extremity injury in the PED within 1 month prior to the interview. A health disparities framework including clinical encounters, health care system factors, provider factors, and patient factors, was derived from extant literature and used to guide the interviews. Interviews were conducted and recorded via Zoom. Open-coding and Nvivo software were used to conduct thematic analyses of participants’ responses.
Results: A total of 10 interviews were conducted among 5 female and 5 male clinicians. Half identified as White, 30% Asian, 10% Black, and 10% Hispanic. Major themes included: race/ethnicity, culture, education, and resources; knowledge, attitudes, and bias; provider communication and cultural competence; and health care organizational culture and quality improvement.
All clinicians identified that patients are treated differently based on race and ethnicity within both the general healthcare system and the PED. All clinicians identified time and systemic issues as barriers to quality care. Other barriers included power dynamics between the clinician and team as well as between the patient and clinician. When asked about possible and personal practices to mitigate bias, prominent themes included (5+ clinicians mentioned) being intentional about verbal and nonverbal communication with families, empathy, and collaborative care amongst clinical teams. The majority (80%) were able to identify feasible and immediate solutions to mitigate bias within the PED.
Conclusion(s): These clinician interviews provide valuable insight into possible solutions to improve patient trust and communication within the healthcare system as well as subsequent resources necessary to eliminate health inequities. Future studies are needed to identify and implement effective interventions.
.jpg)