Mental Health
Mental Health 3
717 - Prevalence and Risk Factors for Depression Among Parents of Children Born Preterm: A Systematic Review and Meta-Analysis of The Evidence Since 2000
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 717
Publication Number: 717.328
Publication Number: 717.328
Megan Moorhouse, University of Manitoba, Winnipeg, MB, Canada; Piranavi Jeyagaran, University of Saskatchewan, Saskatoon, SK, Canada; George N. Okoli, Max Rady College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada; James Bolton, Max Rady College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada; Nicole Askin, WRHA Virtual Library, Winnipeg, MB, Canada; Kristene Cheung, University of Manitoba, Winnipeg, MB, Canada; Deepak Louis, Max Rady College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada; Allan Garland, University of Manitoba, Winnipeg, MB, Canada; Lisa M. Lix, University of Manitoba, Winnipeg, MB, Canada

Megan Moorhouse, MD, Bsc (she/her/hers)
Pediatric Resident
University of Manitoba
Gonor, Manitoba, Canada
Presenting Author(s)
Background: Previous systematic reviews on parental depression following preterm birth were restricted to mothers within the first year after delivery.
Objective: We aimed to systematically review the prevalence and risk factors of depression among mothers and fathers in the first five years following preterm birth.
Design/Methods: Peer reviewed, observational studies, identified through a systematic search strategy of the following databases [Embase (Ovid), Web of Science Core Collection (Clarivate), CINHAL with full text (EBSCOhost), PsycINFO and the Cochrane central], July 2021, were independently screened by two reviewers for eligibility. Studies assessing the prevalence and risk factors for depression among parents of children born preterm (defined as birth < 37 weeks gestation) in the first five years following preterm birth were included. The National Institutes of Health (NIH) quality assessment tool was used for assessing study quality. Meta-analysis using inverse variance effects models were performed.
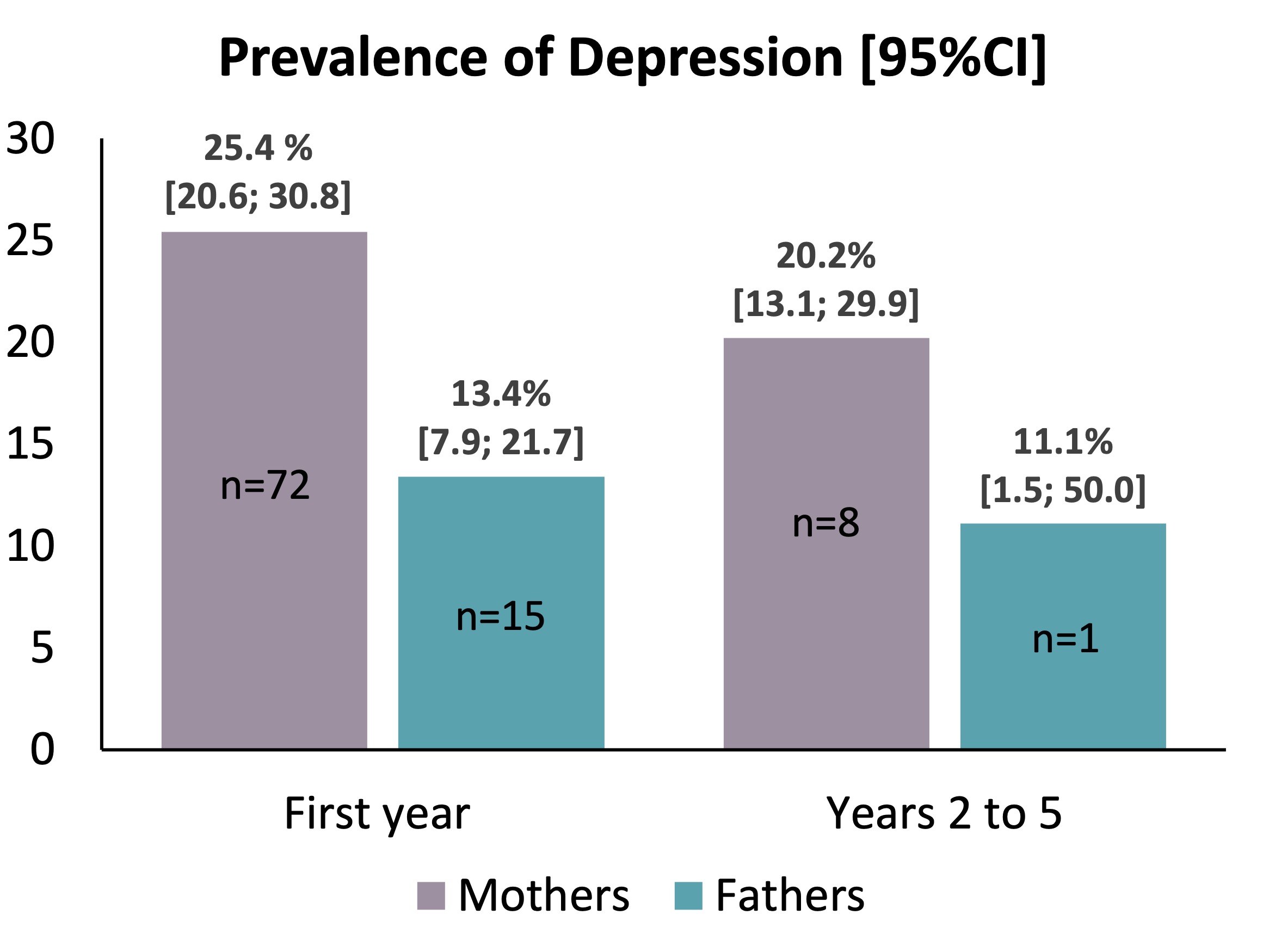
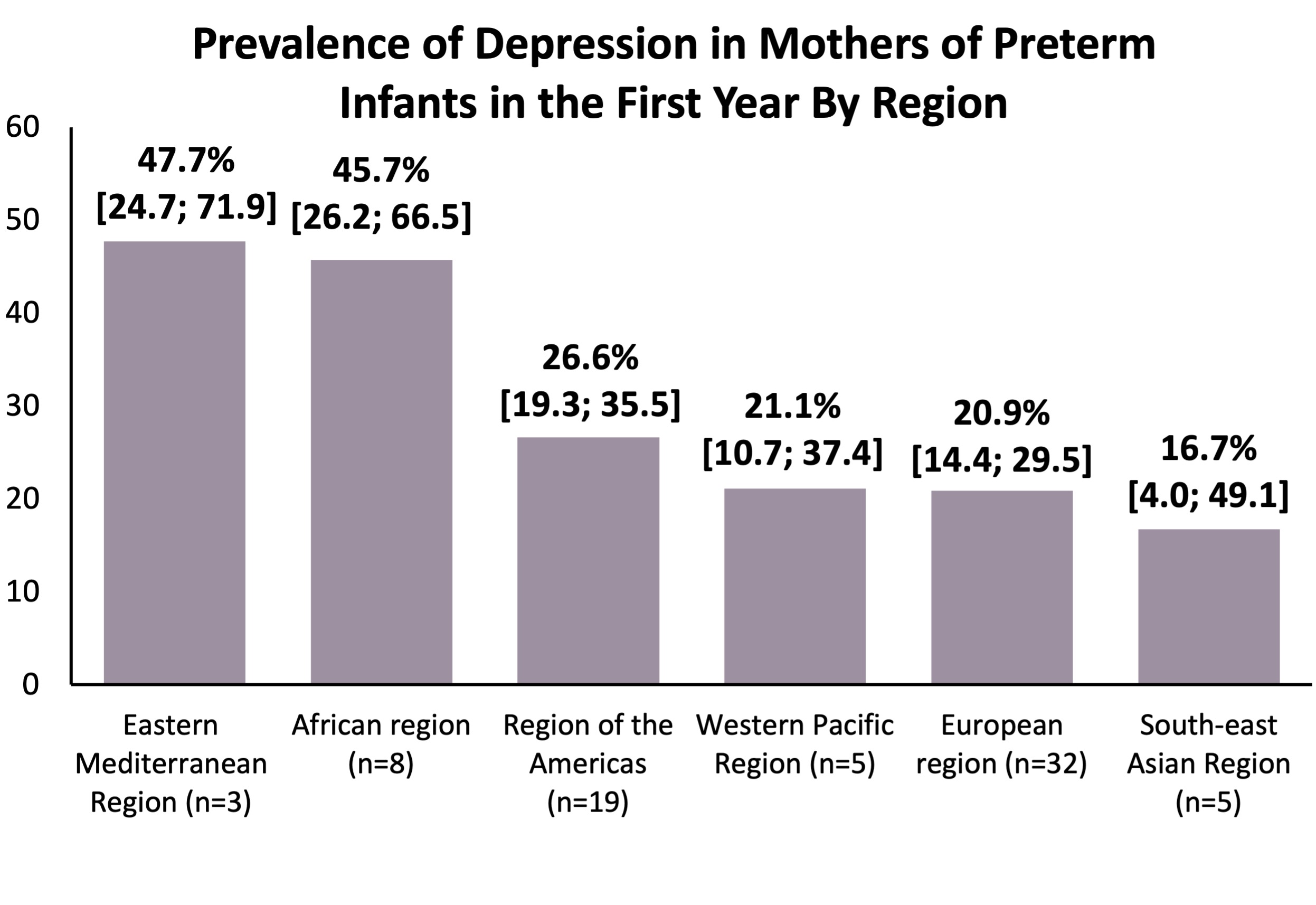
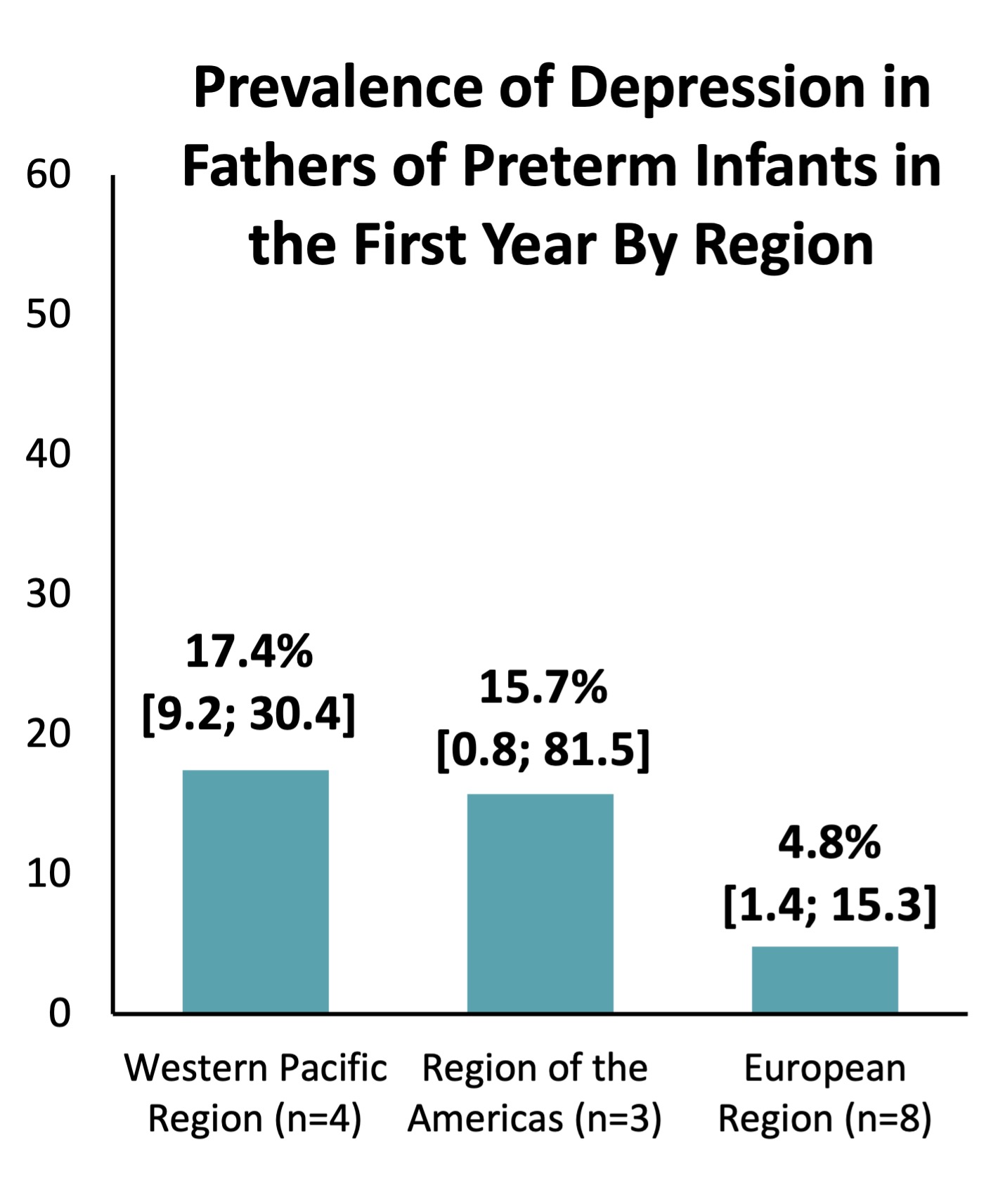
Results: Seventy-eight studies were included. The majority were English language (n=65), European (n=32), cross-sectional (n=44), hospital-based recruitment (n=60) studies and used Edinburgh Postnatal Depression Scale (EPDS) (n=46) to evaluate depression among parents. The prevalence of depression among mothers in the first year of life (n=72) was 25% (95% CI, 21%-31%) and 20% (95% CI, 13%-30%) in years two through five (n=8), while for fathers, they were 13% (95% CI, 8%-22%; n=15) and 11% (95% CI, 2%-50%; n=1) respectively. Mothers from the African and Eastern Mediterranean regions and fathers from the Western Pacific regions had a higher prevalence of depression compared to other regions. Low educational status (OR 3.5 (95%CI, 1.9-6.5; p< 0.0001; I2 = 0%)) significantly increased the risk of depression among mothers in the first year.
Conclusion(s): Mothers and fathers of preterm infants have a high prevalence of depression, with region specific variation in the rates. Low educational status was a risk factor for maternal depression. Limitations of the study include single reviewer translation of non-English articles, heterogeneity among included studies and insufficient data to complete subgroup analysis based on gestational age. This review was registered in Prospero, Registration # CRD42021260748