Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 6
663 - Racial Disparities in Continuity of Care at Pediatric Academic Primary Care Clinics
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 663
Publication Number: 663.317
Publication Number: 663.317
Margaret N. Jones, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Ebunoluwa Falade, University of Cincinnati College of Medicine, Cincinnati, OH, United States; Ilana Primack, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Chunyan Liu, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Lauren M. Lipps, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Shelley Ehrlich, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Andrew F. Beck, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Kristen A. Copeland, Cincinnati Children's, Cincinnati, OH, United States; Mary Burkhardt, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Dominick J. DeBlasio, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Alexandra Corley, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States

Margaret N. Jones, MD FAAP (she/her/hers)
Academic General Pediatrics Fellow
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Continuity of care is associated with improved health outcomes. Black patients have been shown to have less continuity. Additionally, continuity is less common in academic teaching clinics. The Usual Provider Continuity Index (UPC) is a common measure of continuity, defined as the number of visits a patient has with their primary provider divided by their total number of visits. The median UPC in academic clinics from a 2018 review was 0.56. To our knowledge, no studies have assessed demographic disparities in continuity rates at academic clinics.
Objective: To quantify rates of continuity and assess for racial disparities in continuity rates in a set of large pediatric academic clinics.
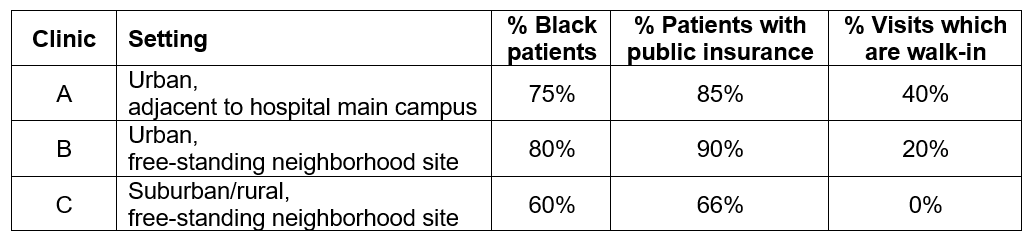
Design/Methods: We conducted a retrospective cohort study. Patients 12-24 months seen at 3 pediatric academic primary care clinics (Table 1) for any visit October 1-31, 2021 were included in our cohort. We then reviewed continuity for these patients in the preceding 12 months (October 1, 2020-October 31, 2021). Patients with less than 2 total visits were excluded. Outcomes included each patient’s UPC for all visits, as well as a modified UPC for well child checks only (UPC Well). Primary covariates included race, ethnicity, insurance, and primary clinic site. We additionally controlled for age, sex, having a care manager, seeing a social worker at any visit, or belonging to our institution’s Medicaid accountable care organization. We evaluated for differences in outcomes by clinic site and patient demographics using bivariate analyses and multivariable regression models.
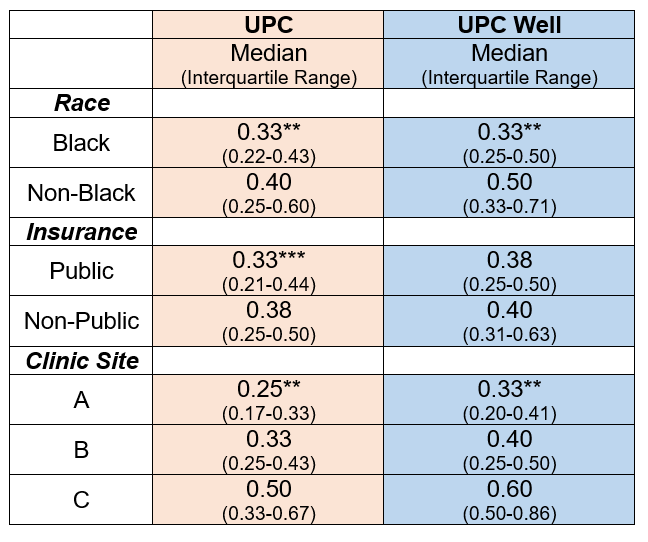
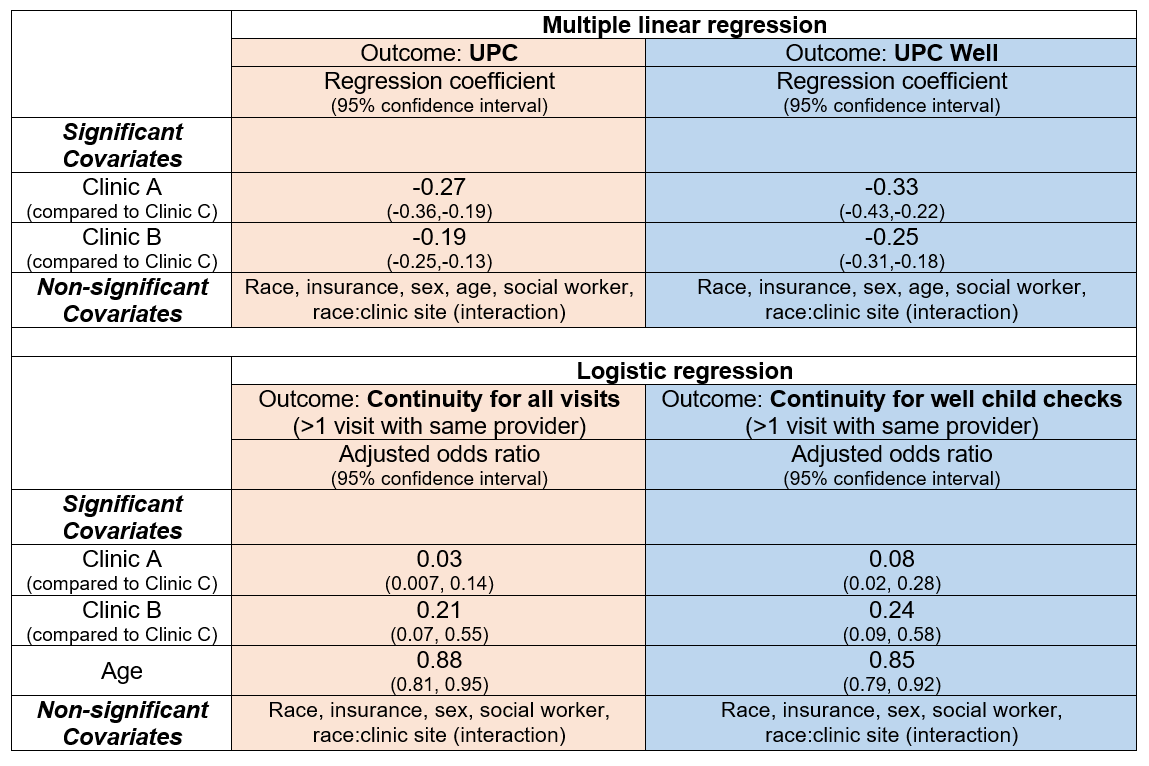
Results: Our cohort included 356 patients (74% Black, 5% Hispanic, 85% public insurance, 52% female, median age 15.8 months). The median UPC was 0.33 and median UPC Well was 0.40. Black patients had lower median values for UPC (0.33 Black vs 0.40 non-Black, p< 0.0001) and UPC Well (0.33 Black vs 0.50 non-Black, p< 0.0001). There were similar disparities in continuity rates by insurance and clinic site (Table 2). In multivariable models, clinic site was the only significant covariate of differences in continuity (Table 3).
Conclusion(s): Clinic sites serving higher percentages of Black patients had lower rates of continuity. Thus, we believe structural racism contributes to these racial disparities in continuity rates, which may be partially attributed to differences in clinic structure and practices. This is a novel analysis of racial disparities in continuity in academic clinics; such analyses can be used to inform family-engaged, co-produced improvement in clinic processes, as well as to address structural changes.