Emergency Medicine: Quality Improvement
Emergency Medicine 10
467 - Reducing ionizing radiation exposure for pediatric patients with concern for intracranial shunt malfunction through implementation of a clinical pathway with QI methodology
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 467
Publication Number: 467.309
Publication Number: 467.309
Nicole Gerber, Weill Cornell Medicine, New York, NY, United States; Sergio W. Guadix, Weill Cornell Medicine, New York, NY, United States; Nisha Narayanan, Weill Cornell Medicine, New York, NY, United States; Elizabeth K. Weidman, Weill Cornell Medicine, New York, NY, United States; Shari Platt, Weill Cornell Medicine, New York, NY, United States; Stephen Oh, Weill Cornell Medicine, New York, NY, United States; Mark Souweidane, Cornell medicine, New york, NY, United States

Nicole Gerber, MD (she/her/hers)
Assistant Professor of Clinical Emergency Medicine and Clinical Pediatrics
Weill Cornell Medicine
New York, New York, United States
Presenting Author(s)
Background: Intracranial shunt (IS) placement is one of the most common neurosurgical procedures and is associated with high rates of revision. The emergency evaluation of patients with clinical concern for IS malfunction, includes imaging with head computed tomography (CT) and shunt series radiographs (XR).
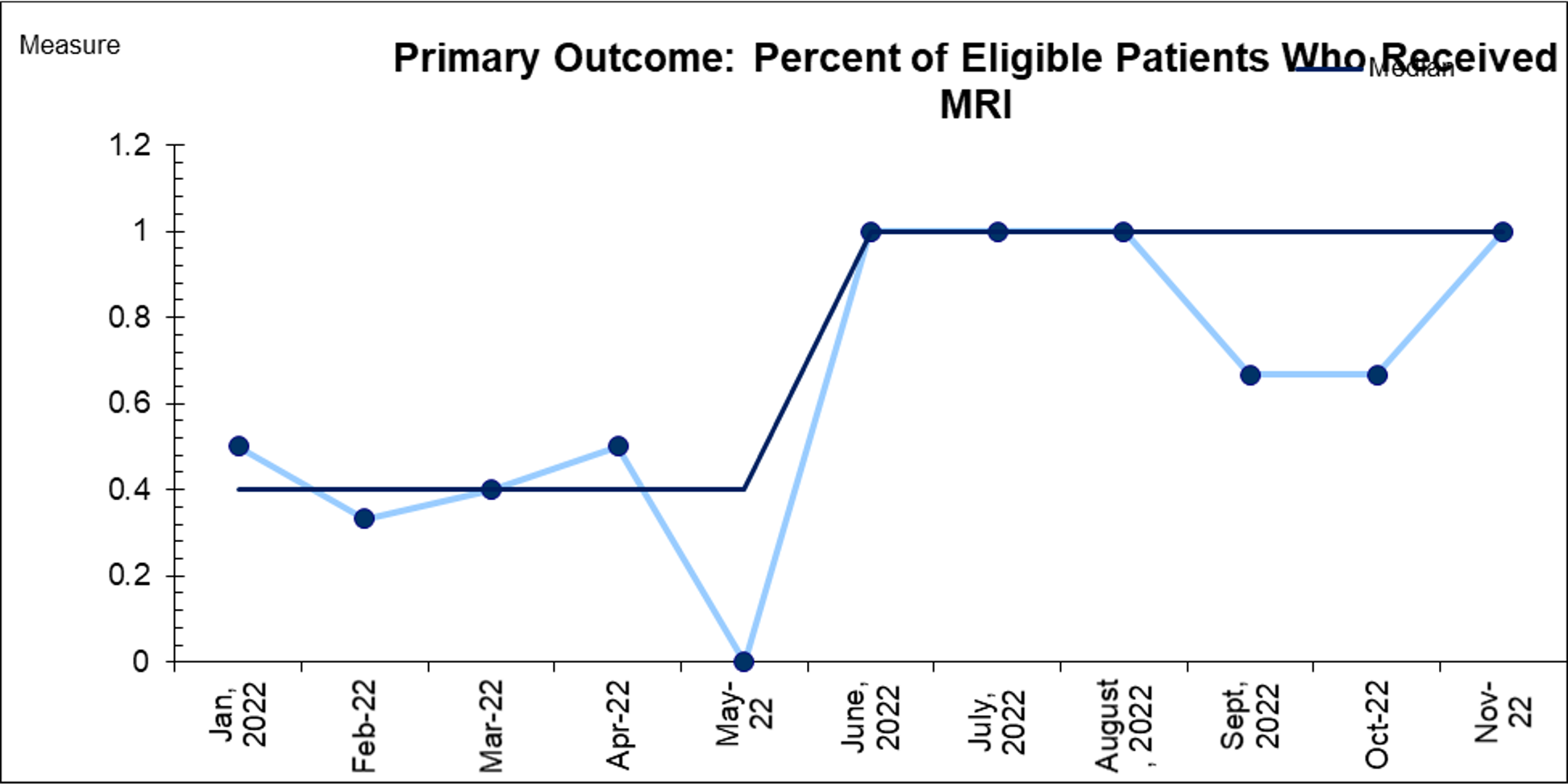
Objective: We aim to reduce exposure to ionizing radiation in children with suspected IS malfunction by increasing use of fast-sequence brain MRI (fsMRI) from 40% to 80% between June 2022 and June 2023.
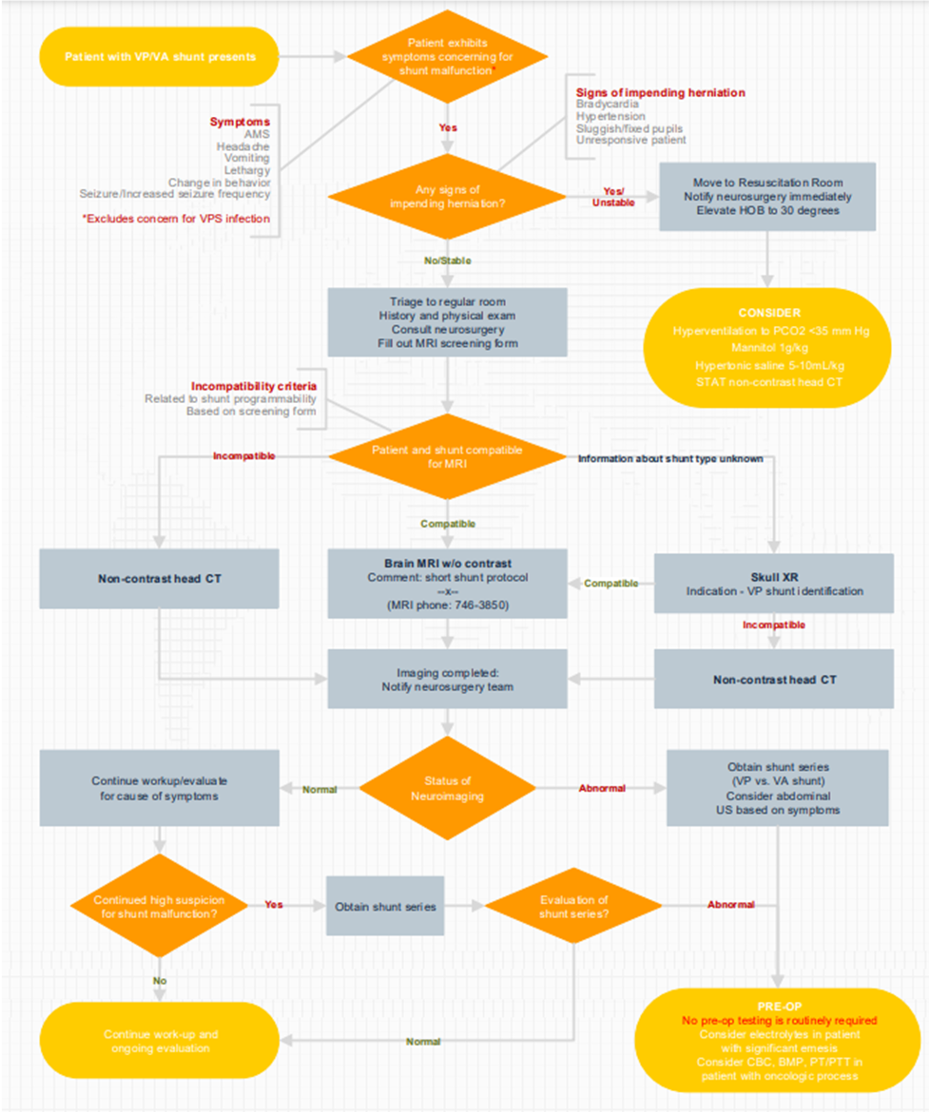
Design/Methods: This ongoing QI project is an observational study with planned sequential experimentation being conducted in the pediatric emergency department (PED) at an urban tertiary care medical center. Key members from pediatric emergency medicine, neurosurgery, and neuroradiology collaborated to develop an algorithm (Figure 1) that prioritizes fsMRI over CT scan in stable pediatric patients with concern for IS malfunction. Patients were ineligible for fsMRI if they were clinically unstable, unable to tolerate MRI previously, or valve information was unknown with concern for reprogramming. This intervention has been tested through three PDSA cycles (launch, reinforcement, expedited MRI processing). Our primary outcome measure is the percent of eligible patients receiving fsMRI and a secondary measure is the percent receiving shunt XR. Process measures include time from arrival to MRI order and completion. Balancing measures include missed IS malfunction, clinical decompensation while awaiting MRI, and PED length of stay (LOS). Measures are gathered via record review. Run charts are utilized to display and analyze the data. Run chart rules are applied to detect signal of change.
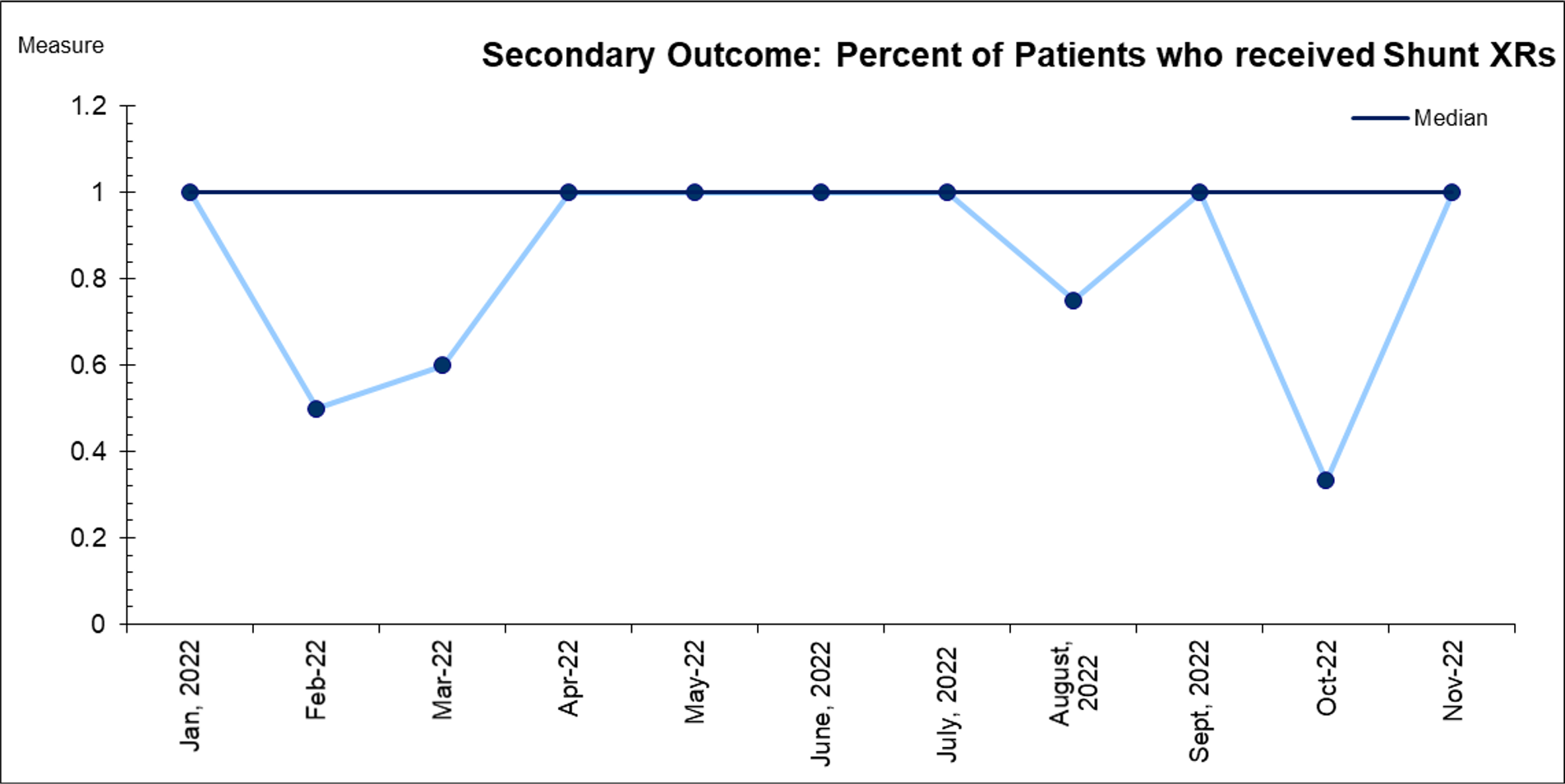
Results: In the 6 months since implementation 25 patients presented to the PED with IS and concern for malfunction. Of 14 eligible patients, 13 (93%) were imaged with fsMRI (Figure 2). The median use of MRI increased from 40% to 100%. Most patients (22/25) received a shunt XR (Figure 3). The average time to MRI order and completion remained unchanged pre- and post-intervention. There were no cases of missed IS malfunction or clinical decompensation while awaiting MRI. ED LOS was unaffected.
Conclusion(s): Implementation of a clinical pathway prioritizing reduced ionizing radiation exposure in children with concern for IS malfunction increased the number of patients receiving fsMRI. There was no change in rates of shunt series XR. Future steps include early MRI ordering and strategies to reduce shunt series XR in select patients.