Emergency Medicine: All Areas
Emergency Medicine 9
454 - Point-of-care lung ultrasound in the emergency department predicts outcomes in bronchiolitis
Publication Number: 454.312

Jaron A. Smith, MD (he/him/his)
Pediatric Emergency Medicine Fellow
University of Texas Southwestern Medical School
Coppell, Texas, United States
Presenting Author(s)
Background:
Acute bronchiolitis (AB) is the most common lower respiratory tract infection in infants and carries significant clinical and financial implications. Objective scoring tools to assess clinical severity and provide disposition guidance have limited application. Additionally, plain film radiography has a minimal role; thus, the gold standard remains entirely clinical. The role of lung ultrasound (LUS) is not well established.
Objective:
1) characterize LUS findings in infants presenting to the pediatric emergency department (ED) diagnosed with AB, and 2) identify associations between the LUS and respiratory support at 12 hours, 24 hours, and maximum during hospitalization; disposition; and length of stay (LOS).
Design/Methods:
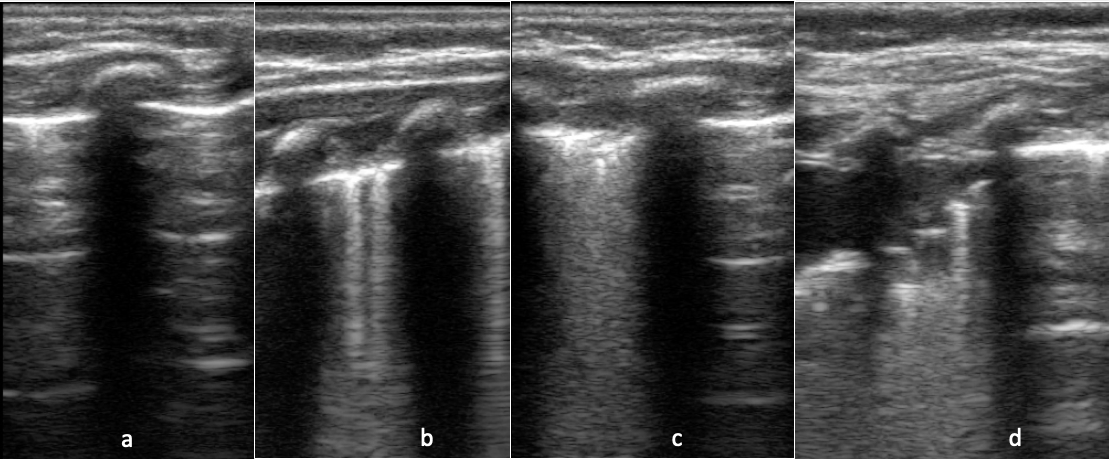
82 infants ≤12 months presenting to the ED and diagnosed with AB were enrolled. LUS was performed at bedside by a physician. Lungs were divided into 12 lung segments and scanned using a lawnmower approach, then scored and summated (min. 0, max. 36) in real time using the following system:
0 - A lines and/or < 3 B lines per lung segment (Figure 1a)
1 - ≥3 B lines per lung segment, but not consolidated or “white out” (1b)
2 - consolidated B lines/"white out”, but no subpleural consolidation or pleural effusion (1c)
3 - subpleural consolidation with any findings in 1b or 1c (1d)
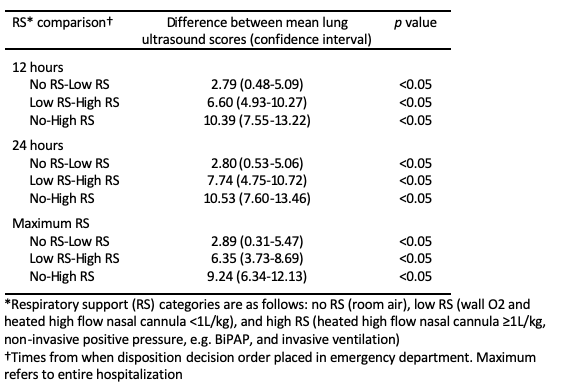
Chart review was performed for all patients after discharge. Respiratory support (RS) was categorized as no RS (room air), low RS (wall O2 and heated high flow nasal cannula (HHFNC) < 1L/kg), and high RS (HHFNC ≥1L/kg and positive pressure including intubation).
Results:
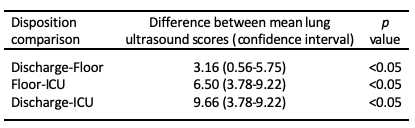
Regarding disposition, the mean (SD) LUS scores were: discharged 1.18 (1.33); admitted to the floor 4.34 (3.62); and admitted to the ICU was 10.84 (6.54). For RS, the mean (SD) LUS scores at 12 hours were: no RS 1.56 (1.93), low RS 4.34 (3.51), and high RS 11.94 (6.17). At 24 hours: no RS 2.11 (2.35), low RS 4.91 (3.86), and high RS 12.64 (6.48). Regarding maximum respiratory support: no RS 1.22 (1.31), low RS 4.11 (3.61), and high RS 10.45 (6.16). The difference between the means for all three dispositions (Table 1) and for all RS time points (Table 2) was statistically significant (p< 0.05).
The mean (SD) length of stay was 84.5 hours (SD 62.9). The Pearson correlation coefficient (r) comparing LOS and LUS was 0.489 (p< 0.0001).
Conclusion(s):
Higher scores on ED-performed bedside LUS for AB are predictive of increased respiratory support, longer LOS, and more acute disposition. The next steps include comparing LUS with clinician gestalt and objective bronchiolitis assessment tools, as well as other LUS techniques.