Medical Education: Simulation & Technology
Medical Education 9: Simulation & Technology 2
520 - Can a digital otoscope be a useful tool for laryngoscopy in practicing pediatric intubations?
Publication Number: 520.327

Pianpian Wu, DO
Pediatric Emergency Medicine Fellow
The Children's Hospital of New Jersey at Newark Beth Israel Medical Center
Newark, New Jersey, United States
Presenting Author(s)
Background:
Airway management during pediatric emergencies is a rare but important clinical skill during resident training. Simulation may be utilized as both a training and assessment tool to teach video laryngoscopy (VL) and direct laryngoscopy (DL) skills. However, VL is not always available for simulation purposes and might not be a feasible financial option in low resource settings. The use of a modified VL in practicing pediatric intubations is limited. The Anykit digital otoscope camera probe is an inexpensive alternative that can be attached to a standard DL blade that may provide an equivalent visualization of the airway.
Objective:
To assess intubation success rate of medical trainees with a custom-made VL versus DL in the simulation setting.
Design/Methods:
In this prospective cohort study, medical trainees participated in simulated endotracheal intubations on the Laerdal SimJunior manikin. The Anykit digital otoscope probe was secured to a 2.0 Miller blade as the custom-made VL. Data collection took place from June to November 2022. Each trainee performed intubation using DL (2.0 Miller blade) followed by the custom-made VL twice. A survey was completed at the end of each session. Primary outcome measures included first attempt success rate and intubation time. Statistical analysis included McNemar tests for categorical variables and Wilcoxon Signed Rank tests for continuous variables.
Results:
A total of 45 participants were recruited, including trainees in Emergency Medicine (n=15, 33.3%), Pediatrics (n=23, 51.1%), Med-Peds (n=4, 8.9%), and Pediatric Emergency Medicine (n=2, 4.4%). First attempt intubation success rate was higher using the custom-made VL (n=39, 86.7%) compared to DL (n=26, 57.8%, p< 0.01). In the second attempt, intubation success rate was higher in both DL (n=39, 86.7%) and custom-made VL (n=44, 97.8%), and intubation times were also faster (p< 0.01). Overall, intubation time was faster in the DL group than the custom-made VL group (p=0.03). Majority of the participants agreed that the simulation was a valuable learning experience (n=43, 95.6%), and that the Anykit otoscope was a useful tool for intubation (n=38, 84.5%). However, there was no clear preference for using VL over DL (p=0.40).
Conclusion(s):
A simulation-based curriculum using a modified VL may improve medical trainees’ competency and success rate with pediatric intubations. The Anykit digital otoscope may be an effective alternative resource in laryngoscopy especially in resource limited settings. Further research should focus on the impact of using a custom-made VL in the clinical setting.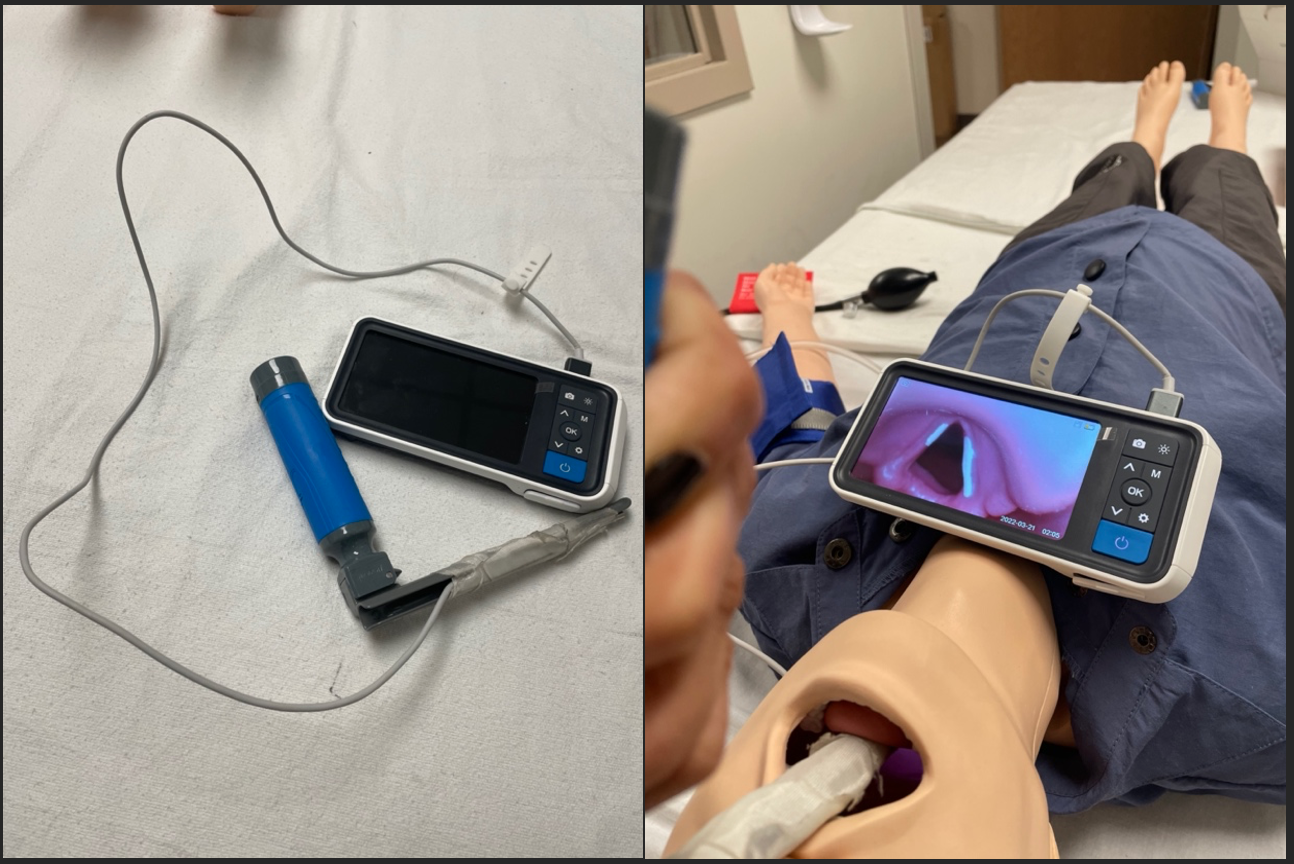
.png)
.png)
