Hypertension
Hypertension 2
25 - Differences in Blood Pressure Severity and Initial Management of Hypertension Disorders in Youth Referred to Pediatric Nephrologists Compared to Pediatric Cardiologists
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 25
Publication Number: 25.322
Publication Number: 25.322
Robert Moy, Levine Children's Hospital, Charlotte, NC, United States; Shupti Biswas, Cohen Children's Medical Center, Floral Park, NY, United States; Aaron M. Bridges, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Wilkesboro, NC, United States; Lucy D'Agostino McGowan, Wake Forest University, Winston Salem, NC, United States; Victoria Giammattei, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, winston-Salem, NC, United States; Margret Kamel, Emory University School of Medicine, Atlanta, GA, United States; Stefan G. Kiessling, Kentucky Children's Hospital, Lexington, KY, United States; Jackson T. Londeree, Emory, Atlanta, GA, United States; Caroline B. Lucas, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Jason Misurac, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States; Margaret Murphy, University of Kentucky College of Medicine, Lexington, KY, United States; Sandeep Riar, Emory University School of Medicine, Atlanta, GA, United States; Christine Sethna, Cohen Children’s Medical Center, New Hyde Park, NY, United States; Andrew M.. South, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States; Irina Viviano, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Donald J. Weaver, Levine Children's Hospital, Charlotte, NC, United States
- RM
Robert Moy, MD (he/him/his)
Pediatric Resident
Levine Children's Hospital
Charlotte, North Carolina, United States
Presenting Author(s)
Background: Youth with hypertension disorders are primarily managed by subspecialists in cardiology or nephrology. Prior literature suggests patients evaluated by pediatric nephrologists are more likely to have more severe hypertension and receive pharmacologic therapy compared to those evaluated by cardiologists.
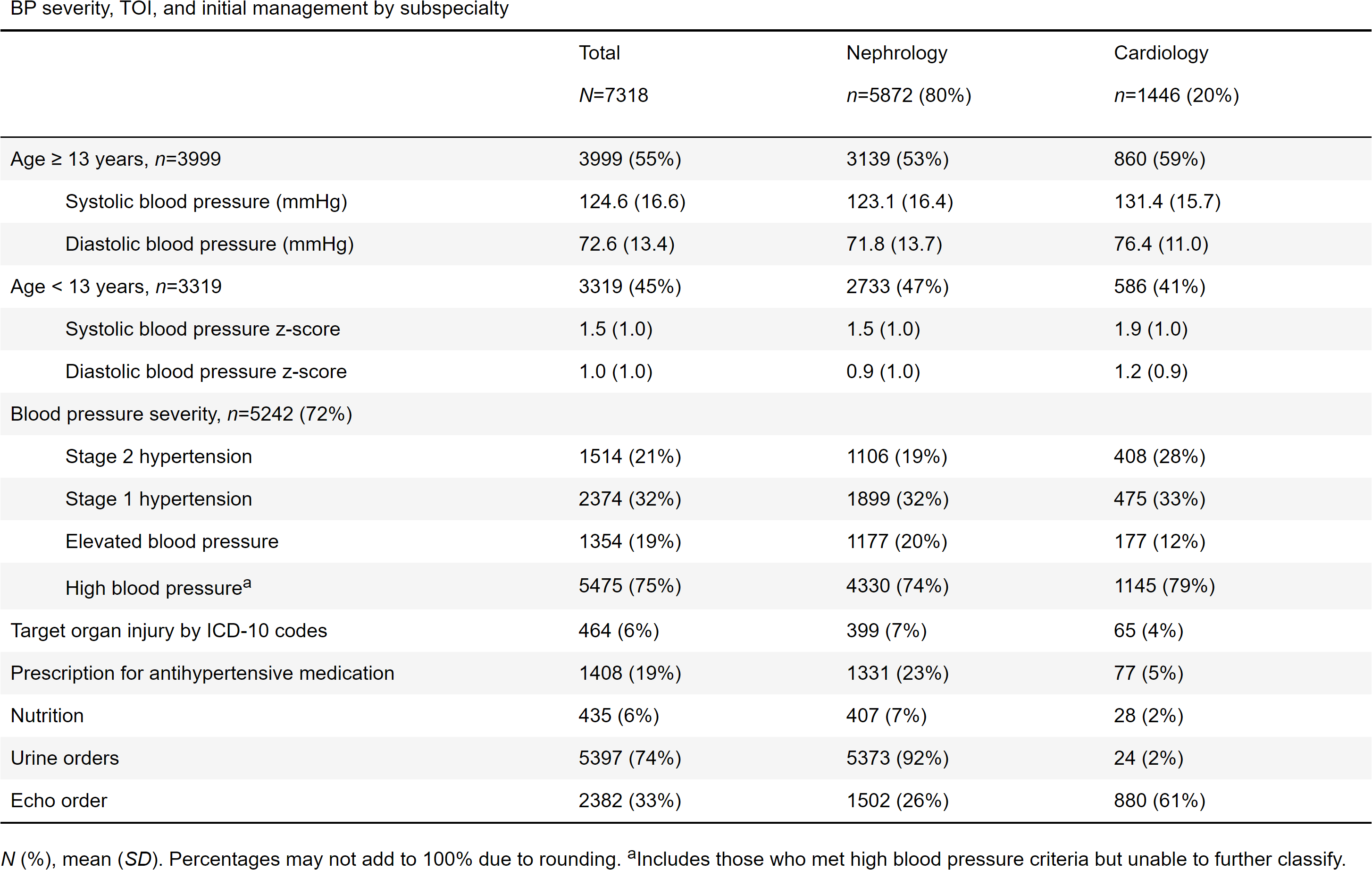
Objective: To investigate if youth referred for hypertension disorders have more severe blood pressure (BP), are more likely to be referred to a dietician, have orders placed to assess for target organ injury, or be prescribed anti-hypertensive medication by nephrologists compared to cardiologists.
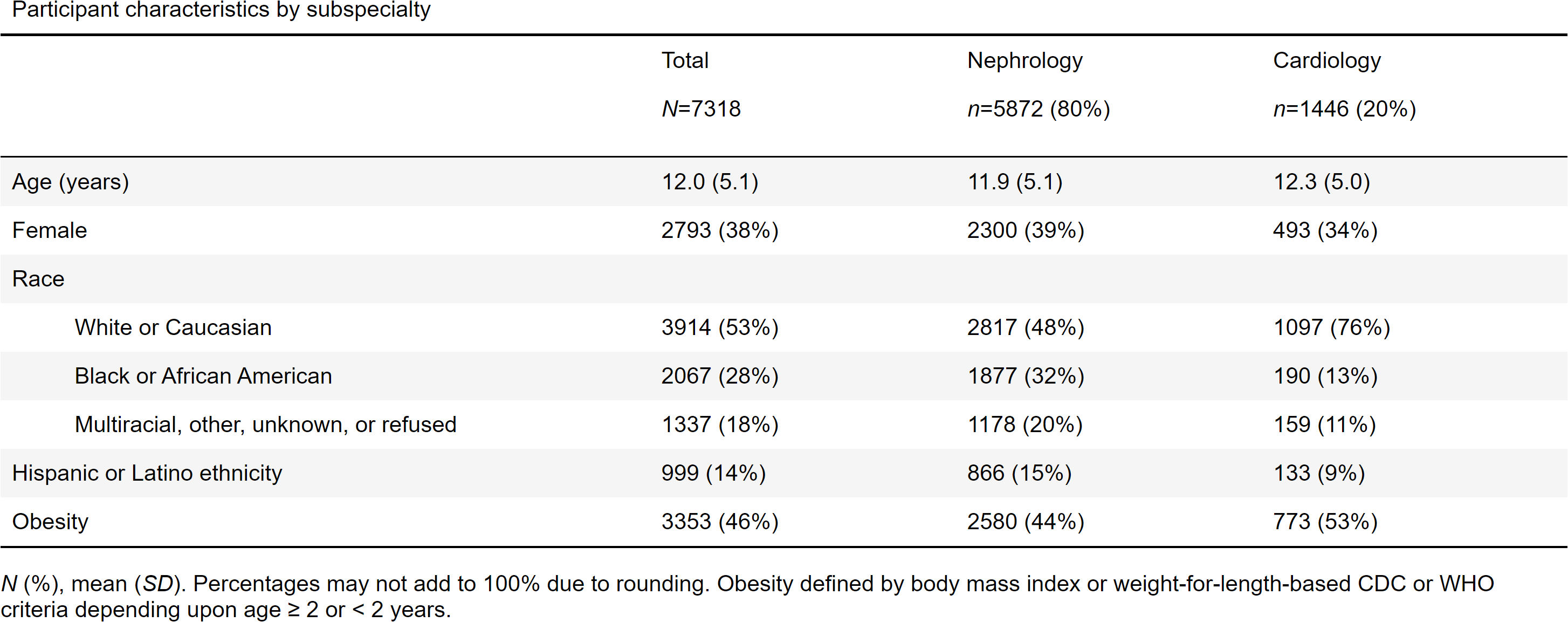
Design/Methods: This is an interim analysis of baseline data from Phase 1.1 of The Study of the Epidemiology of Pediatric Hypertension (SUPERHERO) Registry, a multisite retrospective cohort using electronic health record data. Inclusion criteria were initial visit for hypertension disorder based on ICD-10 codes between 1/1/2015 and 12/31/2021 and age < 19 years. Exclusion criteria were kidney transplant, dialysis, or pregnancy per ICD-10 codes at the index visit. The exposure was referral to nephrology versus cardiology. The outcomes were BP severity and initial management, including orders placed for dietician referral, urine protein or albumin, echocardiogram, and prescription of anti-hypertensive medication. We estimated the associations using unadjusted generalized linear models and Welch Two Sample T-test.
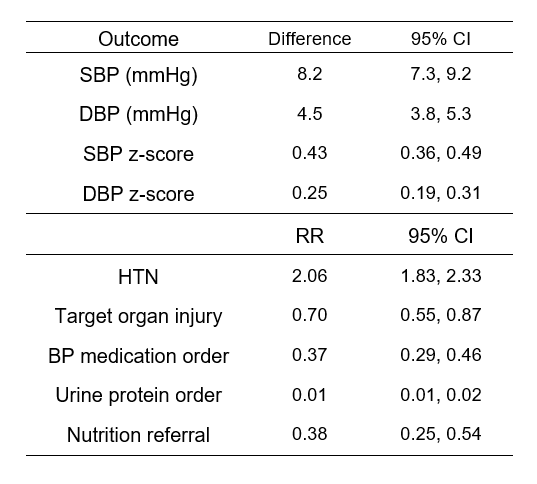
Results: Of 7,318 participants, mean age was 12.0 years, 62% were male, and 53% were Caucasian (Table 1). Patients referred to nephrology were more likely to be non-white or Caucasian (52% vs 24%). BP severity was worse in patients seen by cardiology (+8.2 mmHg, 95% CI 7.3-9.2), but relative risk of target organ injury was lower by generalized linear models (0.70, 95% CI 0.55-0.87). Cardiology was less likely to order urine protein, prescribe antihypertensive medication, or refer to nutrition compared to nephrology.
Conclusion(s): BP was, on average, higher in patients with referrals to pediatric cardiology in contrast with prior literature. Management at time of initial referral also substantially differed regarding diagnostic studies ordered and frequency of antihypertensives ordered, which may have significant implications for quality of care and patient outcomes. Ongoing analysis of the measures that drive these differences is needed to better align care of youth with hypertension by subspecialists.