Asthma
Asthma 1
364 - The Association between Rhinovirus, Respiratory Syncytial Virus or Metapneumovirus Induced Bronchiolitis and Bronchial Hyperresponsiveness and Current Asthma at School-age: Prospective Cohort Study
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 364
Publication Number: 364.302
Publication Number: 364.302
Åsne Myklebust, NTNU - Norwegian university of science and technology, Trondheim, Sor-Trondelag, Norway; Henrik Døllner, Norwegian University of Science and Technology, Trondheim, Sor-Trondelag, Norway; Kari R. Risnes, St Olav University Hospital and Norwegian University of Science and Technology, TRONDHEIM, Sor-Trondelag, Norway

Åsne Myklebust, MD (she/her/hers)
Phd candidate
NTNU - Norwegian university of science and technology
Trondheim, Sor-Trondelag, Norway
Presenting Author(s)
Background: Asthma is the most prevalent chronic disease among school children. Rhinovirus (RV), but also respiratory syncytial virus (RSV), induced bronchiolitis increases the risk for development of asthma. RV-induced early wheezing especially predicts atopic asthma. There are no follow-up data on bronchial hyperresponsiveness (BHR) after bronchiolitis other than RSV. Less is known about lung function and asthma prevalence after metapneumovirus (MPV) bronchiolitis.
Objective: To study BHR and the prevalence of current asthma after bronchiolitis induced by MPV compared to RSV, RV and a healthy control group.
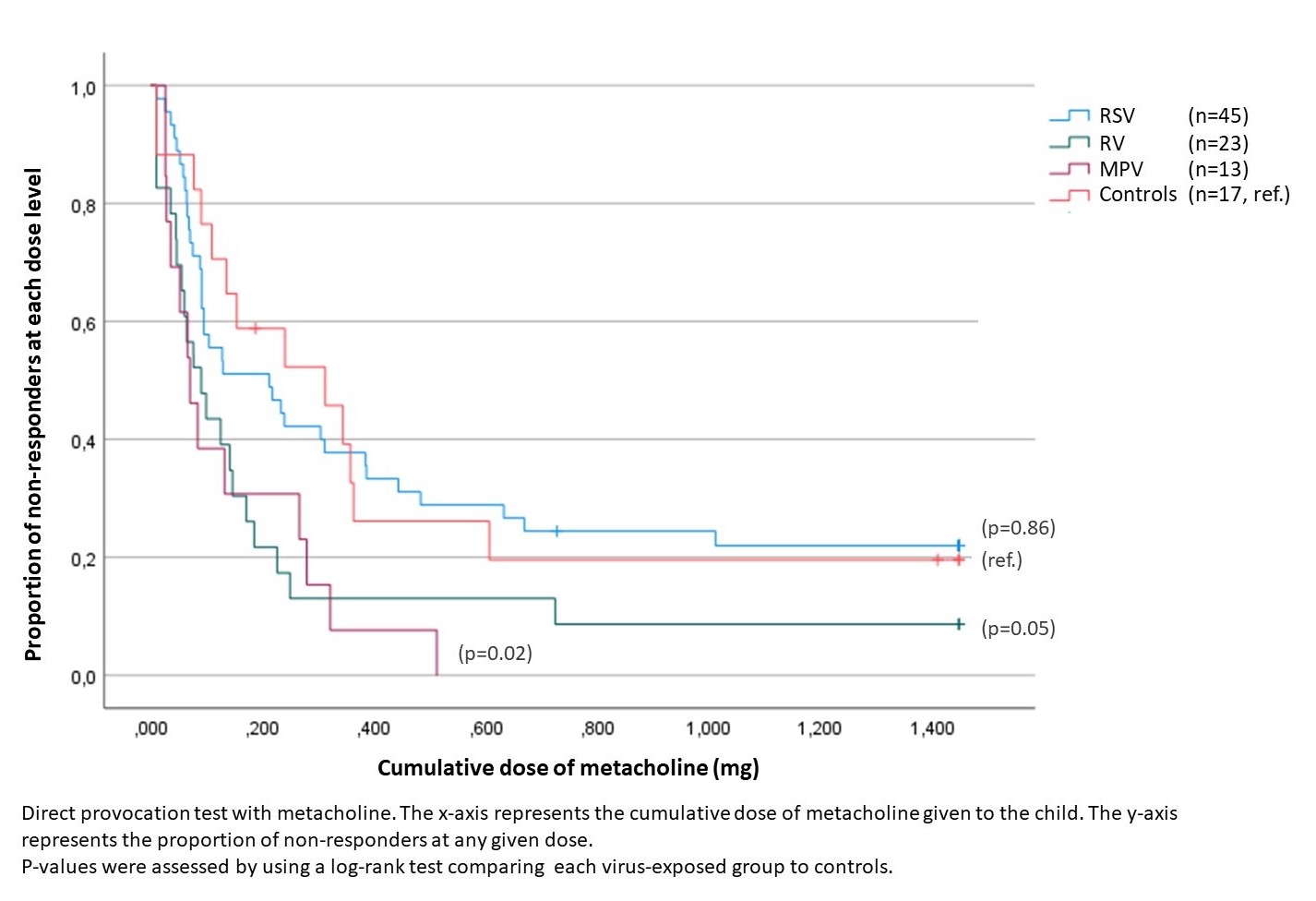
Design/Methods: A cohort of children with viral bronchiolitis at age < 2 years classified by viral exposure (RSV, RV, MPV, mixed infections) and their controls came to follow-up at school age. Systematic clinical assessment and detailed lung function tests including methacholine challenge were performed. The research visit was blinded to viral etiology. Current asthma was defined as typical symptoms plus variable airway obstruction or daily use of inhaled corticosteroids. Allergic asthma required in addition allergen specific IgE sensitization or elevated eosinophils in peripheric blood.
Results: 135 children were included (age range 6-13 years), 51 in the RSV group, 34 in the RV group, 16 in the MPV group, 13 in the mixed infections group and 21 in the control group. Compared to the control subjects, there was increased bronchial hyperresponsiveness to methacholine both in MPV (p=0.02) and RV-infected children (p=0.05) also when quantified as dose-response-slope (p< 0.01 MPV, p=0.01 RV). This was not seen in the RSV group. The prevalence of both asthma (50 % for both MPV and RV) and allergic asthma (29% for MPV and 26% for RV) were higher when compared to RSV (respectively, 43% and 11%) and controls (respectively 24% and 17%).
Conclusion(s): The data indicates that MPV and RV etiology of bronchiolitis, but not RSV, are likely to be associated with increased airway reactivity at school-age. Viral bronchiolitis, especially induced by MPV or RV, is closely linked to later asthma and allergic asthma.
.jpg)
.jpg)