Neonatal Infectious Diseases/Immunology
Neonatal Infectious Diseases/Immunology 4
420 - Inter-alpha Inhibitor Proteins (IAIP) Levels Measured by Enzyme-linked Immunosorbent Assay (ELISA) & Lateral Flow Immunoassay (LFIA) Are Both Reliable Detections of Neonatal Sepsis
Publication Number: 420.335
- RC
Ray Chen, MD
Research Assistant
Women & Infants Hospital of Rhode Island
Brown University
Providence, Rhode Island, United States
Presenting Author(s)
Background:
Inter-alpha Inhibitor Proteins (IAIP) are endogenous serine protease inhibitors
and a novel inflammatory biomarker. We have demonstrated that IAIP levels
decrease after immune activation in animal models and humans. Sepsis is a
systemic inflammatory response to overwhelming infection of the bloodstream.
Early diagnosis and treatment of sepsis are associated with improved outcomes.
Enzyme-linked immunosorbent assay (ELISA) is the standard laboratory procedure
to measure IAIP levels. We developed a quantitative lateral flow immunoassay
(LFIA) that allows rapid measurement of IAIP levels at point of care. We
hypothesized that infants with sepsis have significantly altered IAIP levels,
whether measured by ELISA or LFIA.
Objective:
To compare IAIP levels measured by a standard 6-hour ELISA and a rapid 15-
minute LFIA format in neonates with proven sepsis and controls.
Design/Methods:
A prospective, multi-center, cross-sectional study was conducted. Blood samples
were collected at acute event (clinical decision to take blood culture) and serially
thereafter at 24, 48, and 72 hours. We measured IAIP levels by ELISA (performed
in remote lab) and LFIA (can be performed bedside). We used a linear regression
to compare IAIP levels by ELISA and LFIA and a multivariate logistic regression to
assess associations with infant characteristics and outcomes. Finally we
determined the sensitivity and specificity of LFIA using the receiver operating
characteristic (ROC) curve.
Results:
Thirty-eight infants with sepsis, 22 case controls who had symptoms/signs of
sepsis without a positive blood culture, and 48 gestational age (GA)-matched
controls (Table) were recruited. GA controls had more maternal hypertension and
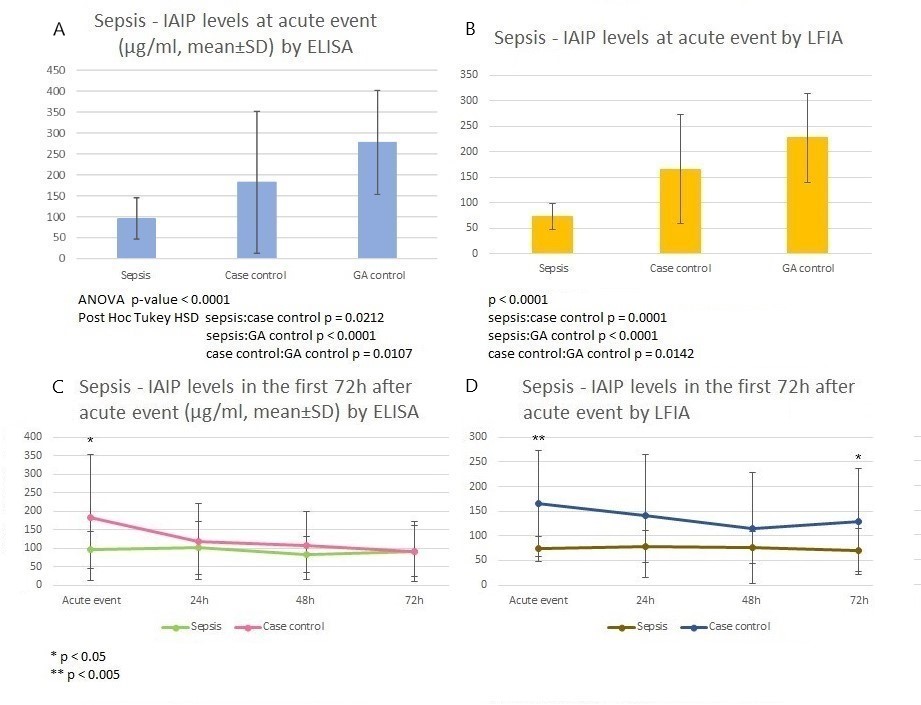
preeclampsia. The multivariate logistic regression showed IAIP levels at acute
event (ELISA and LFIA) and 72 hours after acute event (LFIA) were significantly
reduced in infants with sepsis (Figure 1) after controlling for GA (p-value < 0.05,
R2 = 0.35). IAIP levels by ELISA and LFIA were highly correlated (R2 = 0.94). The
area under curve (AUC) of the ROC analysis for LFIA to detect sepsis was 0.991
with the sensitivity of 96.3% and specificity of 94.6% at a cutoff value of 121
µg/ml (p < 0.001, Figure 2).
Conclusion(s):
Significantly decreased IAIP levels in infants with sepsis suggest activation of the
neonatal systemic response to severe infection. IAIP levels measured by ELISA and
LFIA are both reliable for detection of sepsis. The simple point of care IAIP LFIA is
potentially useful for a rapid detection of sepsis.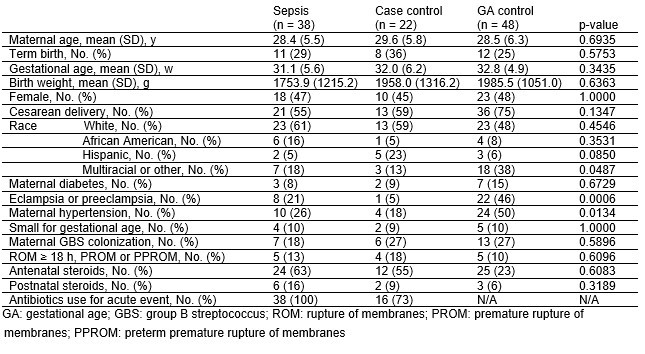
.jpg)
