Emergency Medicine: Quality Improvement
Emergency Medicine 10
464 - Improving pain score documentation and decreasing time to pain medication administration to trauma patients in the emergency Department.
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 464
Publication Number: 464.309
Publication Number: 464.309
Olamide Olabamiji, Case Western Reserve University School of Medicine, Broadview Heights, OH, United States; Tracy McCallin, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Ann M. Bacevice, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Michael Dingeldein, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Nadine M. Berg, UH Rainbow Babies & Children's Hospital, Medina, OH, United States

Olamide Olabamiji, MBBS (she/her/hers)
Pediatric Emergency Medicine Fellow
Case Western Reserve University School of Medicine
Broadview Heights, Ohio, United States
Presenting Author(s)
Background: Pain control in pediatric patients has always been recognized but seemingly undertreated. Pain is often underestimated due to the inadequate assessment tools and the failure to account for wide range of developmental stages.
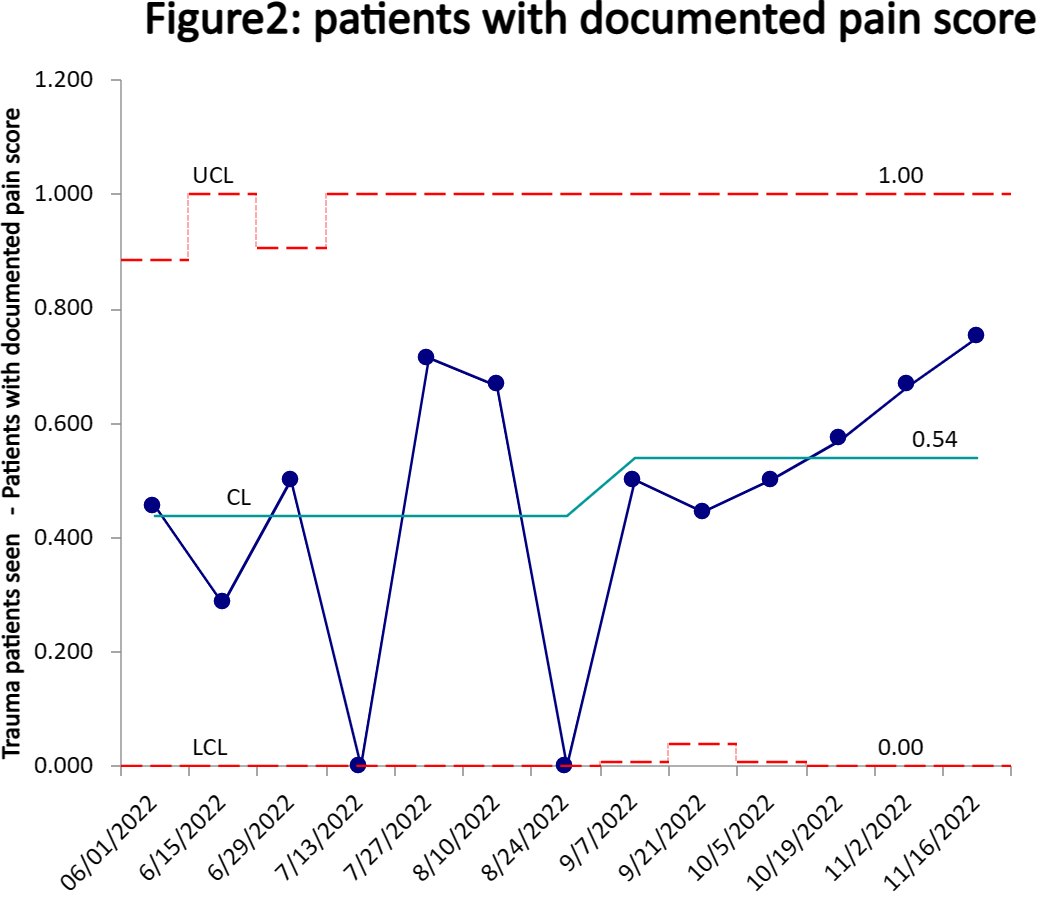
Objective: Data analysis of trauma patients at our institution in 2018, showed time to analgesics of 60 minutes. We reevaluated pain management post-COVID and found 49% of patients had documented pain scores. Our QI goal is to increase pain score documentation to 75% and decrease time to pain medication by 15% over 3 months.
Design/Methods:
Using the Model for Improvement, we identified stakeholders, barriers and key drivers for success. Baseline data was gathered for 12 weeks and 3 PDSA cycles from September-November 2022 was done. Data was collected from our institution’s trauma database. Patients who met criteria for full or limited trauma activations were evaluated excluding patients: with pain score less than 5, who received analgesic prior to arrival, without documented pain score, and those intubated/unresponsive or dead. Our intervention utilized a standardized trauma flowsheet including pain score documentation and time to pain medication. Through PDSA cycles, ED staff were educated on pain control in trauma patients, verbal and email reminders, laminated cards posted in the ED and trauma bay. Across all cycles, trauma core nurses did chart audits to ensure timely pain assessment/score documentation.
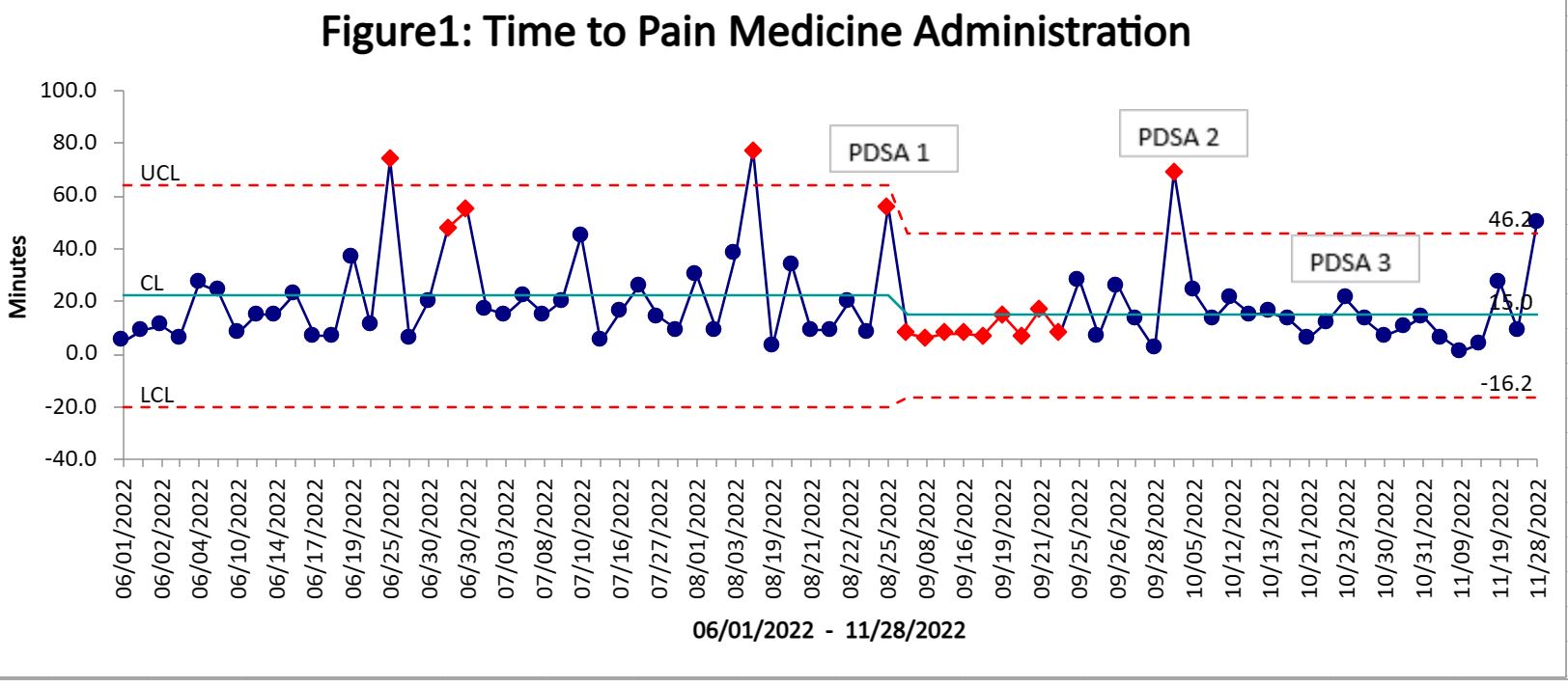
Results: Out of 104 patients, 74 met our criteria after applying exclusions. Baseline data showed pain score documentation of 45% with average time to pain medication of 22 minutes. At the end of our PDSA cycles, time to pain medication improved to an average of 15 minutes (fig 1), a 30% decrease from baseline, pain score documentation increased to 75% during PDSA 3 (fig 2) both meeting our specific aim.
Conclusion(s): Pediatric pain control has been difficult to measure and inconsistently managed. Our QI project showed improved pain score documentation and decreased time to pain medication. One outlier of 50 minutes to medication, received an analgesic not stocked in the ED. Going forward, we are addressing the diversity of medications available in the ED. A limitation was exclusion of patients receiving analgesics without documented pain score, reducing our total analyzed patients. 3 patients were identified that met criteria for pain medications based on chart review but did not receive analgesics. We are identifying opportunities for improvement with non-documented scores for future PDSA cycles. We also seek to sustain our improved documentation of 75% or higher.