Medical Education: Medical Student
Medical Education 12: Student 2
572 - Therapy and Medical Appointment Utilization Among Medical Students
Publication Number: 572.326

Keats Ewing, MD (he/him/his)
Resident
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background:
Medical student wellness has increasingly become an area of focus and intervention among medical schools to help combat concerning trends of burnout, depression, and suicide. Despite these well-studied trends, there has been little work focusing on if medical students are able to access dedicated resources to emotional and medical wellness.
Objective:
The primary outcome measure was defined as the use of outpatient mental health resources (OMHR) of medical students with subgroup analyses of preclinical versus clinical years of medical school and comparison to utilization of other medical appointments.
Design/Methods: We conducted a cross-sectional, population-based, survey of medical students at an academic medical center. This anonymous, voluntary, self-reported, survey was completed remotely and distributed through the class list-servs and via the respective class group pages. Inclusion criteria included all those currently enrolled at said medical school. Exclusion criteria excluded those who did not want to participate in said survey. For analysis, we used Pearson’s chi-square test for categorical variables to determine whether there were significant differences in outpatient mental health service usage between various subgroups with significance as defined as p < 0.05. This study was reviewed and approved by the Institutional Review Board (IRB).
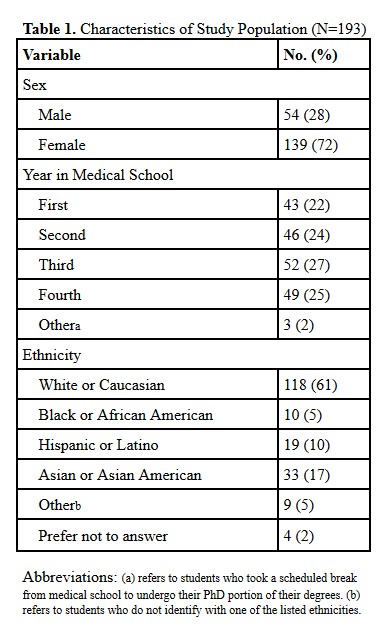
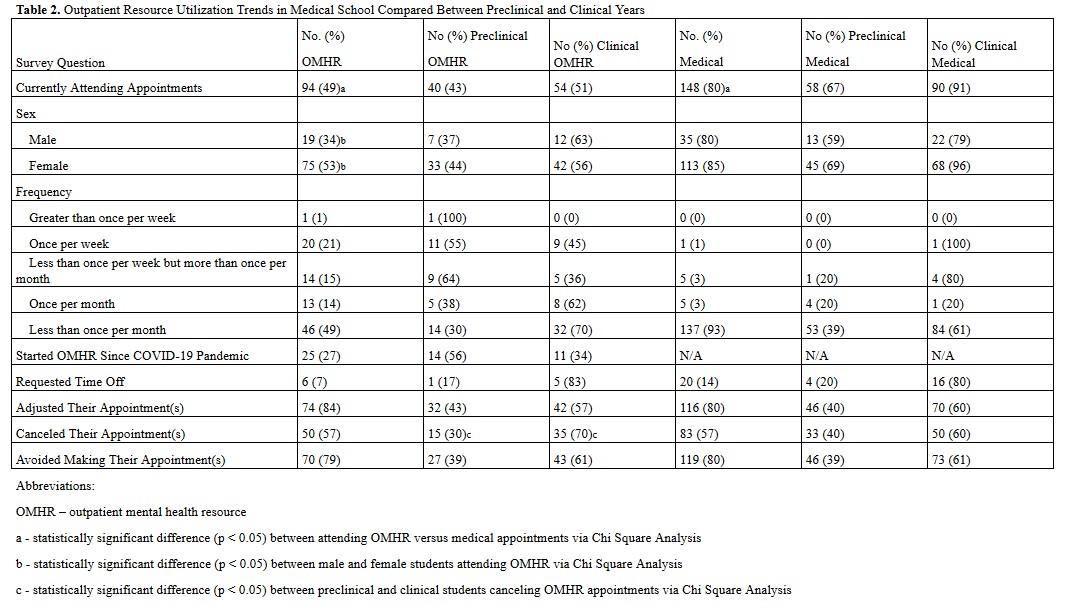
Results: Of 699 medical students available for participation, 27.9% (n = 193) completed the questionnaire and 49% (n = 94) stated they had utilized OMHR at some point during medical school (Table 1). Of those, 57% (n = 50) reported canceling OMHR appointments due to mandatory medical school requirements. In comparison, 80% (n = 148) attended a medical appointment after starting medical school while 57% (n = 83) had to cancel medical appointments. In our subgroup analysis, there was no significant difference in OMHR utilization between students in preclinical versus clinical years (p > 0.05), but those in their clinical years were significantly more likely to cancel OMHR appointments than those in preclinical years (p < 0.05). There was not a significant difference in canceling medical appointments during preclinical versus clinical years (p > 0.05). Women were significantly more likely to attend OMHR appointments than men (p < 0.05), but there was no significant difference between men and women in attending medical appointments (p > 0.05) (Table 2).
Conclusion(s):
The authors’ findings support the need for further medical school administrative support of students as they attempt to receive the emotional and medical wellness they are seeking.