Asthma
Asthma 1
356 - Association between Participation in an Asthma Learning Collaborative and Pediatric Asthma-related Emergency Department Visits
Publication Number: 356.302
- NB
Naomi S. Bardach, MD MAS (she/her/hers)
Professor of Pediatrics and Health Policy
UCSF Benioff Children's Hospital San Francisco
SF, California, United States
Presenting Author(s)
Background:
Quality improvement (QI) efforts can improve guideline-recommended asthma care processes in the pediatric office setting.
Objective: We sought to assess whether participation in a primary care asthma QI collaborative was associated with decreased asthma-related emergency department (ED) visits.
Design/Methods:
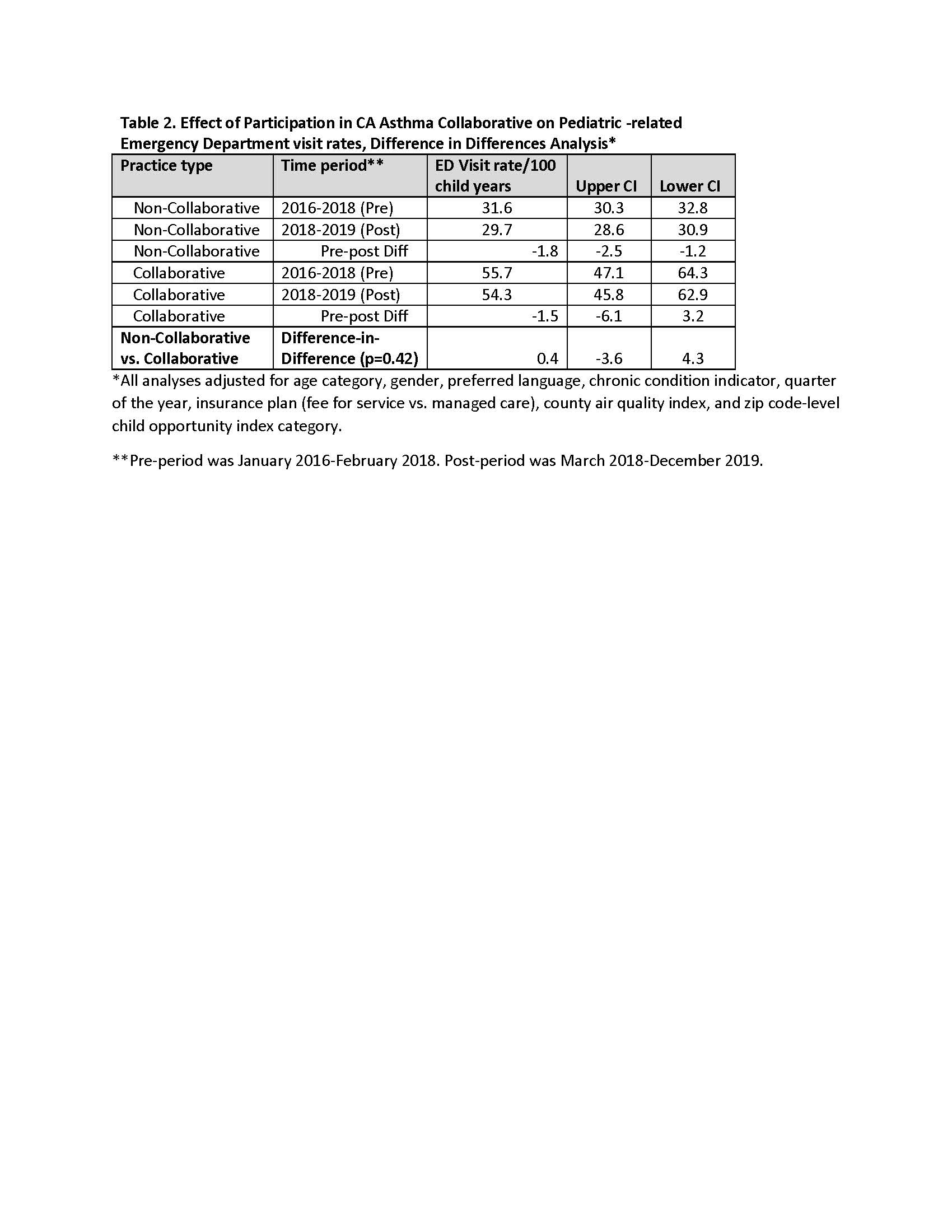
Across 6 northern, central, and southern California (CA) counties, 9 practices participated in a pediatric asthma QI collaborative from 3/2018-12/2019. Collaborative activities included monthly meetings with data review, and plan-do-study-act cycles focusing on guideline concordant care, such as asthma severity assessment, controller medication prescription, smoking screening and cessation counseling, and asthma follow-up visits. Using CA Medicaid claims, we evaluated asthma-related ED visit rates/100 child-years for children 3-21 years with asthma seen by collaborative providers compared to rates for other pediatric asthma patients living in the same counties. We used a difference-in-differences approach with mixed-effects negative binomial regression models controlling for patient (age, gender, insurance, preferred language, chronic condition indicator) and geographical (child opportunity index, air quality index) covariates, and season. Our main analysis measured ED visit rates before (1/2016-2/2018) and after (3/2018-12/2019) the QI collaborative, for patients at participating practices versus other patients in the clinics’ counties. Sustainability during 2020 was not assessed due to COVID-19 pandemic health services disruptions.
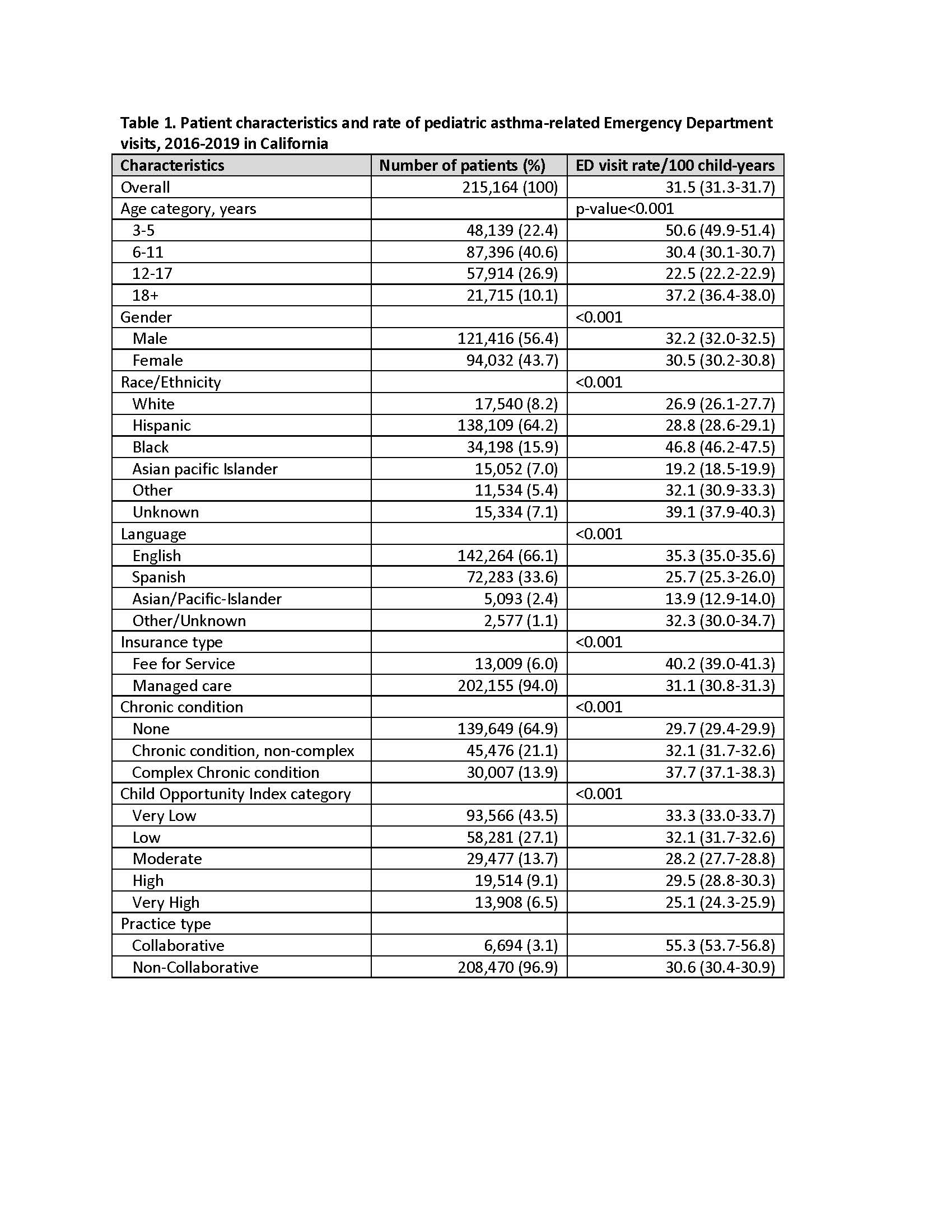
Results: In 215,164 pediatric patients with asthma, there were overall 31.1 asthma-related ED visits/100 child-years. Rates varied substantially by patient characteristics and were higher in collaborative patients (Table 1). Rates decreased across time periods in both collaborative and non-collaborative patients. Rates decreased more for non-collaborative patients (-2.6, 95% CI: -3.3, -1.8)) compared to those seen at collaborative practices (-1.9, 95% CI: -6.5, 2.8). The difference-in-differences (0.7, 95% CI: -3.2, 4.6) was not statistically significant (p=0.24) (Table 2).
Conclusion(s): Participation in an asthma-focused QI collaborative was associated with decreased asthma-related ED visit rates, but the decrease was similar for patients not affiliated with collaborative practices. It is possible that there was not sufficient time to see an effect of collaborative practice changes, as prior studies have seen changes in ED rates a year after improved asthma practices, or that a newly convened collaborative required more time to fully implement practice changes.