Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension 2
234 - Predicting effectiveness of drugs used for treating circulatory failure in preterm infants
Publication Number: 234.33

Maria Carmen Bravo, PhD,MD (she/her/hers)
Consultant Neonatologist
La Paz University Hospital
Madrid, Madrid, Spain
Presenting Author(s)
Background:
Circulatory failure (CF) is a common risk factor for the development of brain and intestinal injury in newborn infants. Cardiovascular support (CVS) for treating this condition has shown modest effectiveness and therapeutic failure is associated with worse prognosis.
Objective: We aim to develop a predictive algorithm for the therapeutic effectiveness of CVS using machine learning techniques.
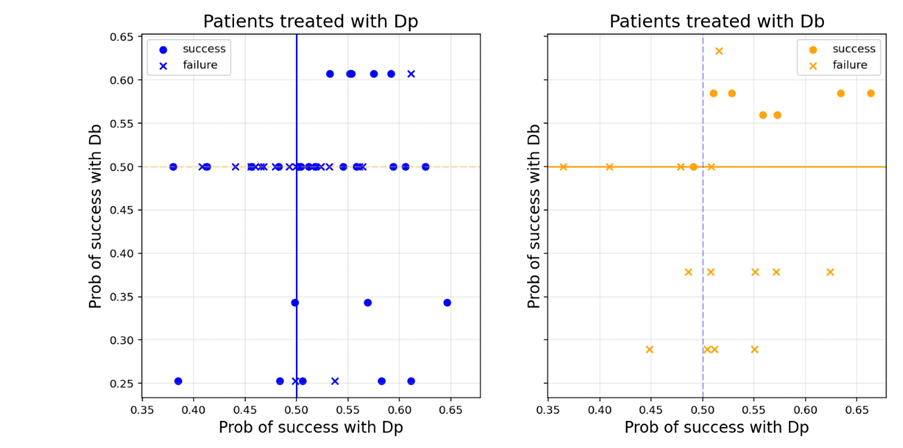
Design/Methods: The medical charts of the infants born between 2017-2020 with a birth weight < 1500 g (VLBW) who had no congenital heart defects and received either dopamine (Dp) or dobutamine (Db) as first line CVS, were reviewed. Treatment response was defined as systolic, diastolic or mean arterial blood pressure increase at least above the third centile for gestational age or SVC flow > 55 ml/kg/min and improving serum lactate or improving negative base excess without adding any other CVS during 24 hours after starting the treatment. A predictive model on the effectiveness of each drug (Dp and Db) to overcome CF (treatment response), fed with an electronic database including demographic, perinatal, clinical and echocardiographic variables, was developed by artificial intelligence techniques. The impact of CVS effectiveness on survival free of gut (necrotizing enterocolitis or spontaneous intestinal perforation) or brain (intraventricular haemorrhage or white matter damage) morbidity was also analysed.
Results:
66 VLBW infants received either Dp (n=44) or Db (n=22) [median gestational age 27.3 (IQ 25-75: 25.3-28.7) weeks; median birth weight 864 (IQ 25-75: 641-1071) g]. Treatment response with the initial CVS was shown in 50% of the cases (Dp 59% and Db 31%, p=0.06). Machine learning techniques identified that a logistic regression model using L1 regularization for Db (top performance over 90%), and L2 regularization or random forests for Dp (top performance 61.4 %), achieved the best predictions, respectively. Sixteen infants died (9% in the treatment response group; 39% in the treatment failure group; p=0.004). Survival free of brain or gut morbidity was more frequently observed in the treatment response (52%) than in the treatment failure (30%) group, p= 0.08.
Conclusion(s):
Lack of CVS effectiveness increases the risk of poor outcome in VLBW infants. The proposed model is able to predict Db therapeutic response with high accuracy so it could be used to assist the clinicians during the decision-making process. Dp effectiveness is hard to predict even with machine learning techniques.