Medical Education: Resident
Medical Education 10: Resident 3
544 - Needs Assessment of Pediatric Senior Resident Readiness to Lead Inpatient Family-Centered Rounds: A Pilot Study
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 544
Publication Number: 544.324
Publication Number: 544.324
Gowry Kulandaivel, University of Utah School of Medicine, Salt Lake City, UT, United States; Pamela Carpenter, Association of Pediatric Program Directors, West Jordan, UT, United States; Erin Avondet, University of Utah School of Medicine, Salt Lake City, UT, United States

Gowry Kulandaivel, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
University of Utah, Primary Children's Hospital
Salt Lake City, Utah, United States
Presenting Author(s)
Background:
The ACGME and ABP utilize Entrustable Professional Activities (EPAs) as competency-based developmental outcomes to assess whether graduating pediatric residents can function without supervision. Evaluation of senior resident leadership skills during inpatient family-centered rounds (FCR) determines achievement of EPA 15: “Lead an Interprofessional Health Care Team”. Few studies, however, have explored how pediatric residencies prepare residents to demonstrate this competency.
Objective:
The study objective is to identify specific educational needs of senior residents to better prepare them to act as team leader during inpatient FCR.
Design/Methods: We recruited categorical pediatric PGY-3 residents at a single institution to participate in virtual semi-structured interviews. Two coders used open coding to independently code the first two transcripts. We generated a codebook by comparing codes and resolving disagreements through discussion. A third coder joined the original coders to analyze the remaining transcripts. The 3 coders met frequently throughout the transcript review to revise the codebook. The coders then identified key themes through an inductive approach to thematic analysis. Data collection and analysis were performed concurrently, and additional interviews are in process to reach thematic saturation.
Results:
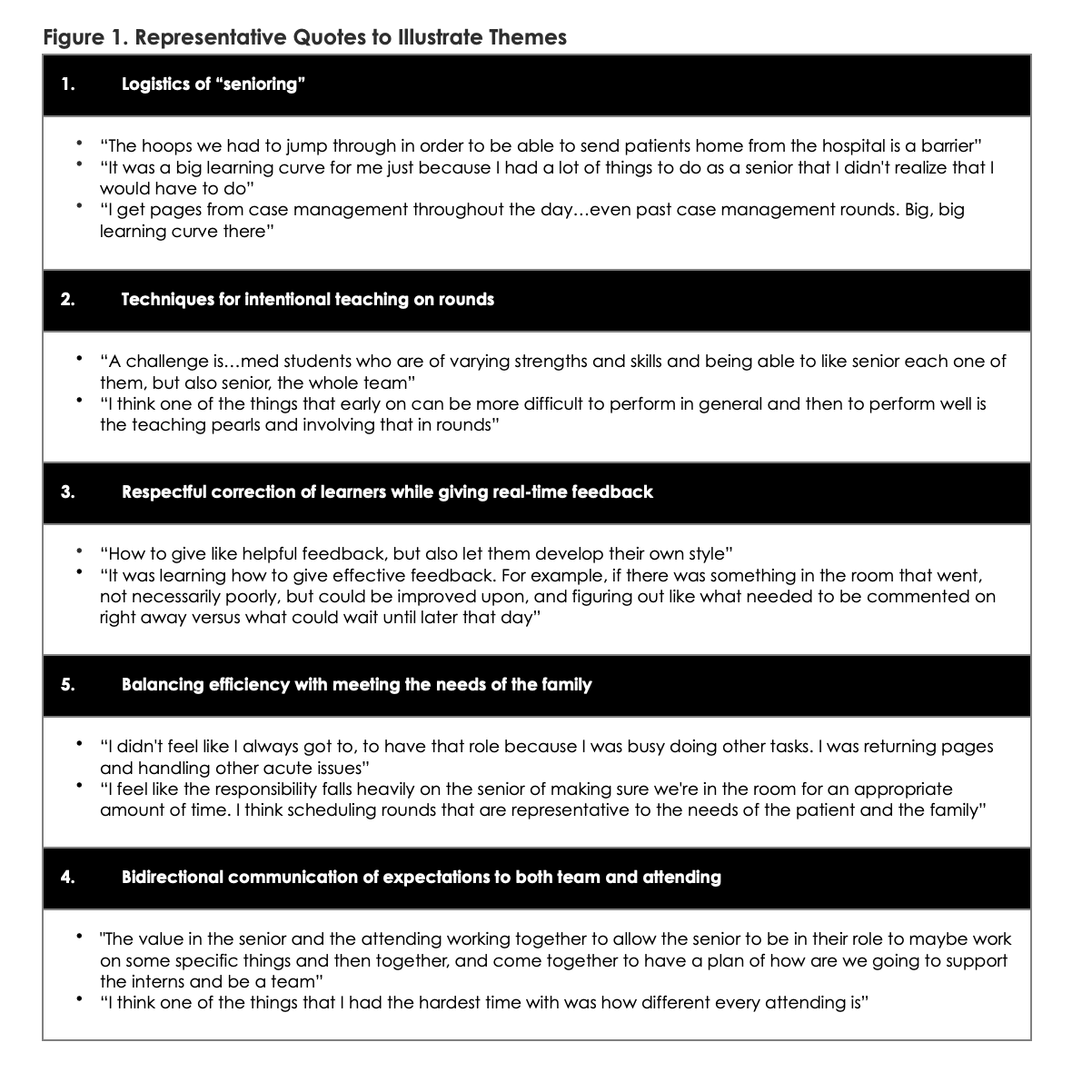
Twelve interviews were completed. Five key themes were identified as educational needs for rising senior residents (Figure 1). (1) Logistics of “senioring” (ex: pre-rounding responsibilities, scheduling rounds, and coordinating discharge with case management). (2) Techniques for intentional teaching on rounds. (3) Respectful correction of learners while giving real-time feedback. (4) Balancing efficiency with meeting the needs of the family. (5) Bidirectional communication of expectations to both team and attending. Residents unanimously reported that instruction on these themes should be delivered through didactics. Organizational and cultural factors, such as competing needs for hospitalist and specialist patients on the same team and varied formats for FCR, emerged as barriers to being prepared to assume the role of a senior resident on inpatient FCR.
Conclusion(s):
Much of the curricular content needed to better prepare senior residents to lead inpatient FCR can be implemented universally across residencies despite structural differences. In contrast, the logistics of senioring are specific to individual residency programs, suggesting that pediatric residencies should explore this teaching domain with their own trainees to augment the universally applicable curriculum.