Children with Chronic Conditions
Children with Chronic Conditions 3
76 - Caregiving Networks for Children with Medical Complexity: A Social Network Analysis Pilot Study
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 76
Publication Number: 76.305
Publication Number: 76.305
Kristina Devi Howell, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Ryan J. Coller, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; HAROLD D. GREEN, Indiana University School of Public Health Bloomingtom, BLOOMINGTON, IN, United States; Patrick Kaminski, Indiana University Bloomington, Bloomington, IN, United States; Elena Alfaro, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Cassandra E. Nelson, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Gemma Warner, Gemma Warner, Madison, WI, United States; Nicole E. E Werner, Indiana University School of Public Health-Bloomington, Bloomington, IN, United States

Kristina Devi Howell, MPH (she/her/hers)
Research Specialist
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background: In homes and communities, children with medical complexity (CMC) are cared for by families and other caregivers, i.e., caregiving networks. Limited research explores network impacts on health or interventions promoting safe and effective caregiving work.
Objective: To determine (1) feasibility of conducting social network analysis (SNA) among CMC caregiving networks, and (2) preliminary associations between network characteristics and hospital use.
Design/Methods: This pilot study recruited primary and secondary caregivers from CMC networks at a large health system. Primary caregivers were parents/guardians of a child with ≥2 complex chronic conditions. Secondary caregivers were identified by primary caregivers, and delivered healthcare, childcare, or resources to families in non-healthcare settings. A CMC network was defined as a primary caregiver and all identified secondary caregivers. Network Canvas software collected interview data. We aimed to enroll 10 primary caregivers and validate responses with up to 2 secondary caregivers per network. Feasibility measures included enrollment, duration, data collection completeness, and ability to calculate network composition, size, centralization, density, and triadic closure. Correlation coefficients explored networks associations with hospital days in the prior year.
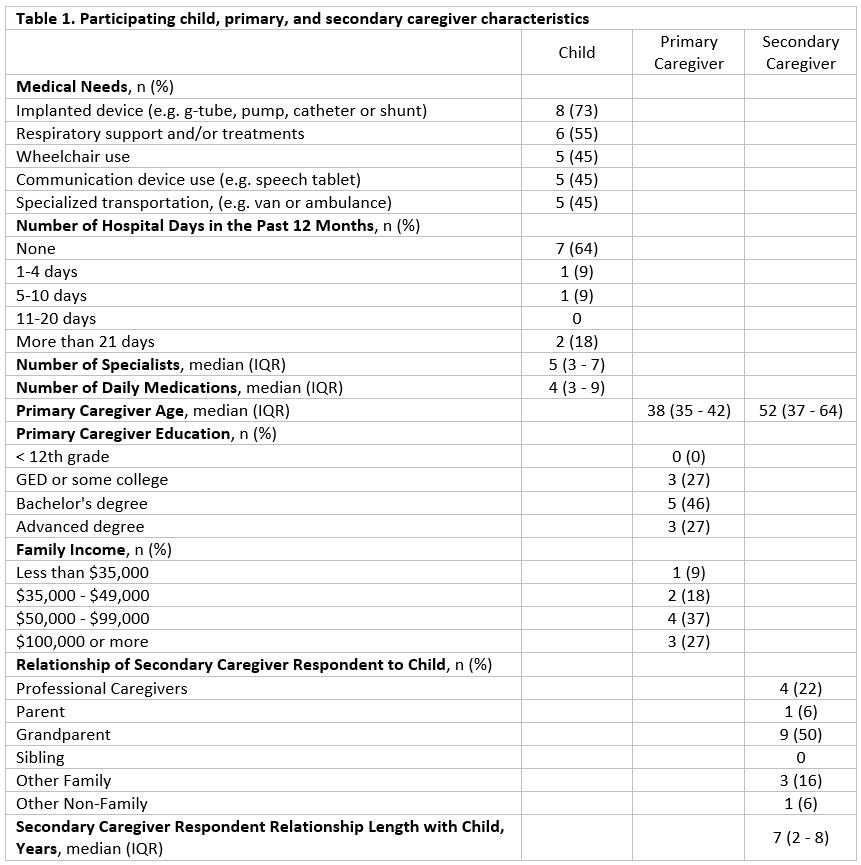
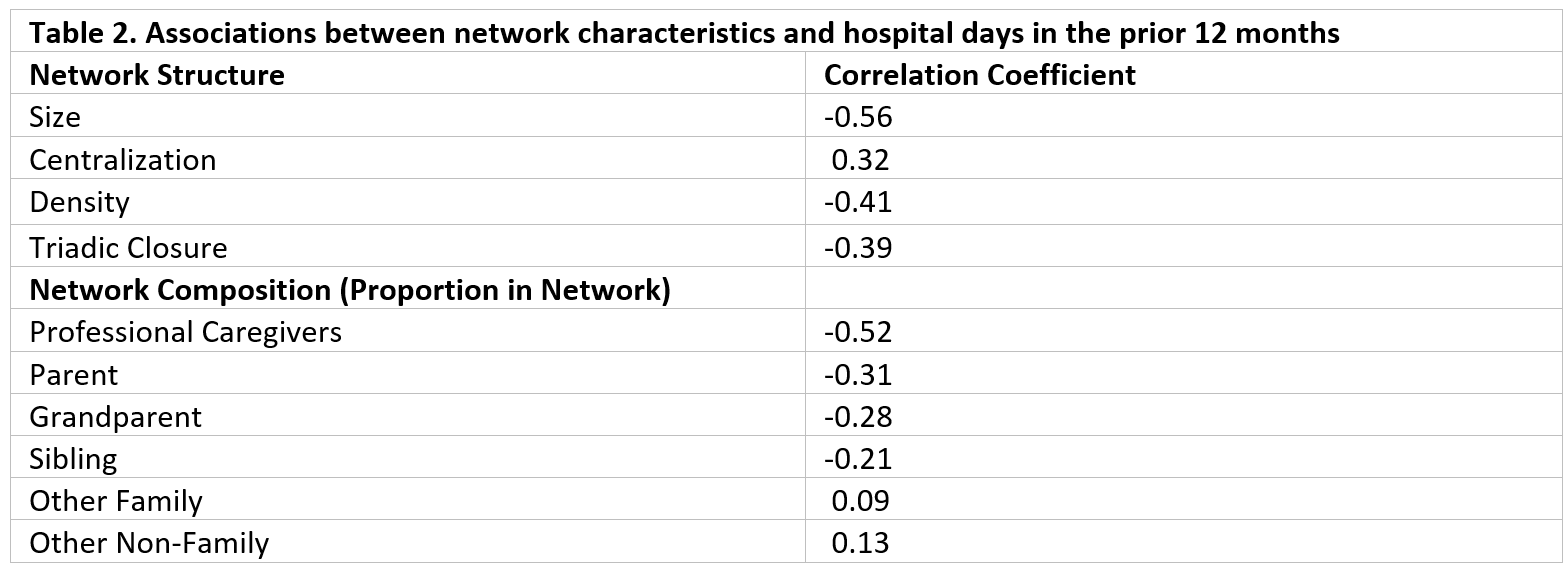
Results: Ten primary and 19 secondary caregivers were recruited in 3 weeks. Table 1 summarizes participant characteristics. Among primary caregivers, 14% declined and 58% of those eligible were enrolled. Among secondary caregivers, 90% were enrolled, with the most frequent roles being grandparents and in-home professionals. Mean (range) network size was 5 (2-12). Mean (range) centralization, density, and triadic closure were 0.21 (0-0.43), 0.53 (0.20-1.00), and 0.57 (0.00-1.00), respectively. Larger, decentralized, denser networks, with more triadic closure, and more professional caregivers correlated with fewer hospital days (Table 2). Fidelity was high with < 1% missing data across all caregivers and study instruments. Study duration for primary and secondary caregivers was < 30 and < 15 minutes, respectively.
Conclusion(s): SNA is a feasible tool to study CMC caregiving networks. Pilot data support hypotheses that CMC network structure and health outcomes are associated. Testing network-based interventions to improve CMC health is an important future direction.